Abstract
In critically ill patients, ventilator-induced diaphragm muscle fibre dysfunction (VIDD) contributes to weaning problems, increasing hospitalisation time and related costs. VIDD pathophysiology remains partially unknown, especially the characterisation of the contractile dysfunction. In the present study, it was hypothesised that Ca2+ activation is affected during VIDD. Ca2+ sensitivity of contraction was therefore evaluated at the single skinned diaphragm muscle fibre level in piglets randomised into sham operation or 5-day mechanical ventilation. Ca2+ sensitivities of force and stiffness in fibres were significantly impaired in all mechanically ventilated piglets compared with sham-operated controls, suggesting a less efficient Ca2+ activation of cells, i.e. a lower relative number of strongly attached cross-bridges for each sub-maximal concentration of Ca2+. In an attempt to test whether this negative effect of VIDD is reversible, single muscle fibres were exposed to the EMD 57033 Ca2+ sensitiser. EMD 57033 (30 µM) improved the Ca2+ sensitivity of force and stiffness in fibres from animals that were mechanically ventilated for 5 days as well as in sham-operated piglets. Thus, EMD 57033 partly restored the Ca2+ activation of cells, reducing VIDD. This finding offers a strong basis for evaluating the effect of Ca2+ sensitisers on diaphragm function in vivo.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Approximately 40% of intensive care unit patients are mechanically ventilated for a median duration of 5 to 7 days [4]; 20% to 30% of these patients experience weaning problems [5]. Weaning failure arises from various factors [40], but is commonly associated with ventilator-induced diaphragm muscle fibre dysfunction (VIDD) [11, 39]. VIDD is characterised by severe fibre atrophy and disrupted contractile function caused by a decrease in fibre maximal force production normalised to cross-sectional area (CSA) [16, 29], i.e. specific force. It is unknown whether other important contractile features are also disrupted, making the knowledge of VIDD pathophysiology incomplete.
In the diaphragm, 18 h of mechanical ventilation is sufficient to induce a down-regulation of myofibrillar proteins synthesis rate [33] and up-regulation of myofibrillar protein degradation [31, 34]. The time course of these changes is faster than in limb muscles where 96 h of unloading is required to induce similar modifications [28]. The generation of reactive oxygen species during mechanical ventilation has an additional damaging effect on existing proteins, including myosin and thin filament elements [43]. Since specific force as well as Ca2+ activation are contractile parameters notably dependent on the proteins content, i.e. myosin [26] and thin filament proteins [23], and on their oxidation status [14, 36], the first aim of the present study was to test the hypothesis that Ca2+ sensitivity of contraction is disrupted in VIDD. The skinned fibre preparation has therefore been used to compare contractile function in single diaphragm muscle fibres from sham-operated control piglets and from piglets mechanically ventilated for 5 days. Force and stiffness were measured at varying Ca2+ concentrations (pCas), ranging from 9.0 to 4.5, to study relative force–pCa and stiffness–pCa relationships and calculate Ca2+ sensitivities of force and stiffness. Because of fibre type-specific contractile behaviour, muscle cells were characterised according to their myosin heavy chain (MyHC) isoform expression. Findings of rightward shifts of the relative force–pCa and stiffness–pCa relationships in fibres expressing the type I and IIa MyHC isoforms confirmed the initial assumption and emphasised the complexity of VIDD pathophysiology.
To date, there is no specific treatment to eradicate or minimise VIDD. Nevertheless, the second objective of the present study was to evaluate the hypothesis that reversing the altered contractile function in VIDD is possible. The use of Ca2+-sensitising agents is a well-recognised effective strategy to restore Ca2+ activation in various conditions [27, 37] and may therefore represent one potential pharmacological intervention strategy in VIDD since Ca2+ sensitisers such as EMD 57033 bind to myofibrillar proteins, commonly thin filament structures, promoting their Ca2+-induced conformation, subsequent cross-bridge formation and overall contractile activation in cardiac [35, 38] and skeletal muscles [13, 18, 27]. Skinned diaphragm muscle fibres from mechanically ventilated piglets were therefore exposed to 30 µM of EMD 57033 to evaluate the effects on the Ca2+ sensitivity of force and stiffness. The leftward shifts of the relative force–pCa and stiffness–pCa curves particularly in type I fibres corroborated the hypothesis.
Materials and methods
Animals
A detailed description of animals has been given elsewhere [25]. Briefly, eight female domestic piglets (23–30 kg body weight) were included. After initial preparation, animals were allowed to rest for 1 h. Prior to induction of anaesthesia, animals were given an intramuscular (i.m.) injection of atropine 0.1 mg kg−1 and azaperon 4 mg kg−1 i.m. for sedation. After arrival in the laboratory, anaesthesia was induced with pentobarbitone 15–20 mg kg−1 administered intravenously (i.v.). During the study period, the animals were carefully monitored and checked 24 h/day for 5 days. They were sedated using isoflurane inhalation (Abbott Laboratories, 0.8–1.3% end-tidal concentration) supplemented by intravenous bolus doses of morphine and ketamine as needed. After induction, the trachea was cannulated via a midline incision, and a trachestomy tube was placed distally to the cricothyroid cartilage. All animals were then mechanically normoventilated using volume-controlled ventilation (Servo 300; Siemens Elema) at a FiO2 of 0.21–0.30 and a respiratory rate of 20 breaths per minute. During the whole study period, the inspired tidal volume was adjusted to 12–15 ml kg−1 to maintain arterial oxygen and carbon dioxide tensions within normal limits. Arterial and central venous catheters were placed in the common carotid artery and the internal jugular vein via a separate incision on the neck and under antiseptic conditions. Arterial and central venous blood pressures, airway pressures, rectal temperature and standard three-lead ECG were continuously monitored. Excessive heat loss was avoided by covering the animals when necessary with a warming blanket. A urinary catheter was placed in the urinary bladder, through a low midline abdominal incision, for continuous monitoring of urinary output. Arterial acid–base balance, oxygen and carbon dioxide tensions, electrolytes and blood glucose concentration were monitored using ABL 2 and OSM2 analyzers (Radiometer) and a Glucometer (Bayer Health Care). A continuous infusion of Ringer's acetate at 2,000–4,000 ml day−1 was given for fluid replacement and to assure a urinary output of 25–50 ml h−1 throughout the study period. All wounds were carefully cleaned and closed by standard sutures to avoid unwanted contamination.
The animals were randomised into (a) a sham-operated control (CTL) group (N = 4) where mechanical ventilation and sedation was applied for 3 h and (b) a mechanically ventilated (MV) experimental group (N = 4) where ventilation was effective for 5 days and accompanied by continuous sedation as described above. In the MV group, animal position was altered daily between the left and right lateral position to improve gas exchange, allow pulmonary secretion to be removed via tracheal suctioning and to avoid pressure wounds. In addition, prophylactic antibiotic (Streptocillin Vet; Boehringer) was administered i.v. once daily. During the 5-day period, nutritional support was provided by a continuous infusion of buffered glucose 2.5 mg ml−1, and the infusion rate was adjusted to maintain a tight control of arterial blood glucose levels at 4–8 mM. No vasopressors or additional fluids were given to any of the animals.
The study protocol was approved by the Local Ethical Committee on Animal Research at Linköping University (Dnr 15/97).
Muscle biopsies and permeabilisation of fibres
Biopsy specimens (2 × 2 cm) from the left anterior costal diaphragm were obtained after abdominal incision prior to euthanising the animal at the end point of the experiment (day 5) for all piglets from the MV group. In the CTL group, piglets were killed at the start point of the experiment (3 h). Biopsy specimen were placed in relaxing solution at 4°C, and bundles of ∼50 fibres were dissected free and then tied with surgical silk to glass capillary tubes at slightly stretched lengths. The muscle bundles were then treated with skinning solution (relaxing solution containing glycerol; 50:50 v/v) for 24 h at 4°C, after which they were transferred to −20°C. The muscle bundles were treated with sucrose, a cryo-protectant, within 1–2 weeks for long-term storage [7]. After the sucrose treatment, muscle bundles were detached from the capillary tubes and snap frozen in liquid nitrogen-chilled propane and stored at −160°C.
Single muscle fibre experimental procedure
On the day of an experiment, a fibre segment 1 to 2 mm long was left exposed to the experimental solution between connectors leading to a force transducer (model 400A, Aurora Scientific) and a lever arm system (model 308B, Aurora Scientific) [22]. The total compliance of the attachment system was carefully checked and remained similar for all the single muscle fibres tested (5 ± 0.5% of the fibre length). The apparatus was mounted on the stage of an inverted microscope (model IX70; Olympus). While the fibre segments were in relaxing solution, the sarcomere length was set to 2.65–2.75 µm (optimal sarcomere length for cells from these animals) by adjusting the overall segment length [15]. The diameter of the fibre segment between the connectors was measured through the microscope at a magnification of ×320 with an image analysis system prior to the mechanical experiments. Fibre depth was measured by recording the vertical displacement of the microscope nosepiece while focusing on the top and bottom surfaces of the fibre. The focusing control of the microscope was used as a micrometre. Fibre CSA was calculated from the diameter and depth, assuming an elliptical circumference, and was corrected for the 20% swelling that is known to occur during skinning [22].
Relaxing and activating solutions contained (in mM) 4 Mg-ATP, 1 free Mg2+, 20 imidazole, 7 EGTA, 14.5 creatine phosphate, and KCl to adjust the ionic strength to 180 mM. The pH was adjusted to 7.0. The concentrations of free Ca2+ were 10−9 M (relaxing solution) and 10−6.2, 10−6.0, 10−5.8, 10−5.5, 10−5.2, 10−5.0 and 10−4.5 M (activating solutions), expressed as pCas (i.e. −log [Ca2+]). Apparent stability constants for Ca2+–EGTA were corrected for temperature (15°C) and ionic strength (180 mM). The computer programme of Fabiato [6] was used to calculate the concentrations of each metal, ligand and metal–ligand complex. EMD 57033 was a gift from Dr N. Beier (E. Merck Pharmaceuticals). It was prepared as a 10 mM stock solution in DMSO and was diluted in relaxing solution to obtain a final EMD 57033 concentration of 30 µM and a DMSO concentration of 0.3% (v/v). Control solutions were prepared with an equivalent volume of DMSO, which had no effect on the fibres.
At 15°C, immediately preceding each activation, the fibre was immersed for 10–20 s in a solution with a reduced Ca2+–EGTA buffering capacity. This solution is identical to the relaxing solution except that the EGTA concentration is reduced to 0.5 mM, which results in more rapid attainment of steady-state force during subsequent activation.
Force
This was calculated as the difference between the steady-state isometric force in activating solutions and the resting force measured in the same segment while in the relaxing solution. Force was adjusted for CSA.
Stiffness
Once steady-state isometric force was reached, small-amplitude sinusoidal changes in length (ΔL ± 0.2% of fibre length) were applied at 500 Hz at one end of the fibre [20]. The resultant force response (ΔF) was measured, and the mean of 20 consecutive readings of ΔL and ΔF was used to determine stiffness. The actual elastic modulus (E) was calculated as the difference between E in activating solutions and resting E measured in the same segment in the relaxing solution. E was determined as follows [21]:
Relative force–pCa and stiffness–pCa relationships
Each fibre was exposed to different solutions with pCas varying from 9.0 to 4.5. Force and stiffness were normalised to maximum force and stiffness at pCa 4.5, allowing the construction of relative force–pCa and relative stiffness–pCa curves. To determine the midpoint (termed pCa50) and the Hill coefficient (nH) from the pCa curves, data were fitted (SigmaPlot 5.0 and Origin 6.1 Professional software; Jandel Scientific) using a three-parameter Hill equation:
Where X is the relative force or relative stiffness, −log[Ca50] is the midpoint (pCa50), and nH is the Hill coefficient.
For contractile measurements, strict acceptance criteria were applied. First, the sarcomere length was checked during the experiments, using a high-speed video analysis system (model 901A HVSL, Aurora Scientific). A muscle fibre was accepted and included in the analyses: (a) if the sarcomere length of a single muscle fibre changed <0.10 µm between relaxation and maximum activation and (b) if maximal force changed <10% from first to final activation [22].
After the mechanical measurements, each fibre was placed in urea buffer (120 g urea, 38 g thiourea, 70 ml H20, 25 g mixed bed resin, 2.89 g dithiothreitol, 1.51 g Trizma base, 7.5 g SDS, and 0.004% bromophenol blue) in a plastic microcentrifuge tube and stored at −80°C.
MyHC isoform expression
The MyHC isoform composition of fibres was determined by 6% sodium dodecyl sulfatepolyacrylamide gel electrophoresis (SDS-PAGE). Sample loads were kept small (equivalent to ∼0.05 mm of fibre segment) to improve the resolution of the MyHC bands. Electrophoresis was performed at 120 V for 24 h with a Tris–glycine electrode buffer (pH 8.3) at 15°C (SE 600 vertical slab gel unit, Hoefer Scientific Instruments). The gels were silver-stained and subsequently scanned in a soft laser densitometer (Molecular Dynamics) with a high spatial resolution (50 μm pixel spacing) and 4,096 optical density levels. Due to the small number of fibres expressing the type IIx MyHC isoform, comparisons were restricted to fibres expressing the type I and IIa MyHC isoforms.
MyHC, MyLC and actin quantification
MyHC, myosin light chain (MyLC)1s/f, MyLC2s/f and actin contents of single fibres were determined by 12% SDS-PAGE (Fig. 1). The acrylamide concentration was 4% (wt/vol) in the stacking gel and 12% in the running gel, and the gel matrix included 10% glycerol. The gels were stained with Coomassie blue (0.5 g brilliant blue, 225 ml MeOH, 225 ml distilled H20, and 50 ml acetic acid). The relative contents were then calculated from the densitometric scanning (see above).
Statistical analysis
A total of 127 diaphragm fibres obtained from four CTL piglets and four MV piglets were used, i.e. a minimum of 15 acceptable fibres per animal. In the present manuscript, data are presented as means ± standard error of the means (SEMs). Sigma Stat software (Jandel Scientific) was used to generate descriptive statistics. A three-way ANOVA \( \left( {{\text{group}}\left[ {{\text{CTL}} - {\text{MV}}} \right] \times {\text{fibre}}\,{\text{type}}\left[ {{\text{I}} - {\text{IIa}}} \right] \times {\text{compound}}\,{\text{treatment}}\left[ {{\text{before}} - {\text{after}}} \right]} \right) \) was applied for each parameter (P 0/CSA, E0, pCa50 of force, nH of force, pCa50 of stiffness and nH of stiffness). In addition, a two-way ANOVA \( \left( {{\text{group}}\left[ {{\text{CTL}} - {\text{MV}}} \right] \times {\text{fibre}}\,{\text{type}}\left[ {{\text{I}} - {\text{IIa}}} \right]} \right) \) was performed for each proteins ratio. In case of differences, the post hoc Tukey test was performed. The level of significance was set at p < 0.05.
Results
After permeabilisation, muscle fibres were isolated from the bundles and mounted for contractile analyses. A total of 127 muscle fibres expressing the type I and IIa MyHC isoforms from the MV and CTL groups fulfilled the criteria for acceptance and were included in the analyses.
VIDD pathophysiology
At pCa 4.5, force normalised to cross-sectional area, i.e. specific force (P 0/CSA), and stiffness (E 0) were lower in both types I and IIa fibres from the MV group than the CTL animals (Table 1). It should be noticed that pCa 4.5 corresponded to maximum activating Ca2+ concentration. In fact, previous data have shown no significant difference between pCa 4.0 and 4.5.
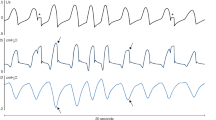
The dependences of force and stiffness on Ca2+ concentration were characterised by two parameters obtained from fitting the data to the Hill equation (see “Materials and methods”), i.e. the pCa required to elicit half of the maximal force production (pCa50 or Ca2+ sensitivity) and the steepness (nH or Hill coefficient; Fig. 2). pCa50 of force was lower for type I and IIa fibres, whereas nH of force was higher solely in type I fibres from MV piglets when comparing with CTL animals (Table 2). pCa50 of stiffness was also lower for type I and IIa fibres and nH higher in fibres expressing the slow MyHC isoform in MV animals compared with CTL piglets (Table 2). Stiffness depends on the number of attached cross-bridges [10], the force/compliance of each cross-bridge and the compliance of the structures in series with the cross-bridges (the thick filament, proteins along the thin filament and probably also Z-disks) [8, 9, 32]. The strong linear relationships between the relative stiffness and the relative force in both mechanically ventilated and control piglets (Fig. 2) suggest that stiffness is primarily dependent on the number of attached cross-bridges at all levels of Ca2+ activation [30].
Otherwise, the MyHC, MyLC1s, MyLC1f, MyLC2s and MyLC2f to actin content ratios were unchanged among fibres expressing the type I and IIa MyHC isoforms (Table 3).
EMD 57033-related changes
At pCa 4.5, P 0/CSA and E 0 were not affected by the exposure to EMD 57033 in both types I and IIa fibres from the MV nor CTL groups (Table 1).
pCa50 of force, on the other hand, increased in type I fibres from MV piglets as well as in type I and IIa fibres from CTL animals (Table 2). The Ca2+ sensitiser did not significantly affect nH of force (Table 2), and it provoked an increase in pCa50 of stiffness in type I fibres from piglets belonging to MV group and in type I and IIa fibres from CTL animals whereas nH remained unchanged (Table 2). The maintained linear relationships (relative stiffness vs. relative force) in mechanically ventilated and control piglets after exposure to EMD 57033 suggest that stiffness remains primarily dependent on the number of attached cross-bridges at all levels of Ca2+ activation also after the treatment with the Ca2+ sensitiser.
Discussion
The results from the animal model emphasise that VIDD pathophysiology in critically ill patients is complex; it is characterised not solely by atrophy and decreased force-generating capacity (specific force) but also by a reduction in the Ca2+ sensitivity of contraction. Results from the present study also demonstrate that some of these modifications are not immutable and can, in part, be counterbalanced, as attested by the increased Ca2+ sensitivities of force and stiffness in fibres exposed to EMD 57033. Under certain conditions, Ca2+ sensitisation may offer a promising mechanism to decrease VIDD and weaning problems.
VIDD pathophysiology
In addition to a dramatic decrease in specific force (Table 1) due to a loss in the total number of strongly attached cross-bridges (Table 1), a significant desensitisation of force production to Ca2+ concentration was observed as indicated by the rightward shift of pCa50 of force in type I and IIa fibres from piglets that were mechanically ventilated for 5 days compared with control animals, i.e. a higher Ca2+ concentration was required to activate the diaphragm muscle cells. This indicates a less efficient regulation of muscle contraction, since Ca2+ sequestration is an energy-consuming process [1]. To investigate whether this striking VIDD feature was due to a change in the number of strongly attached cross-bridges, the relative stiffness–pCa relationship was studied. A lower pCa50 of stiffness was observed in type I and IIa fibres from mechanically ventilated piglets than controls (Table 2), indicating a decrease in the relative number of recruited cross-bridges at each sub-maximal Ca2+ concentration. We have previously observed a similar desensitisation to Ca2+ concentration in limb muscle fibres with a preferential loss of myosin in patients with acute quadriplegic myopathy [26]. However, in the present study, the MyHC, MyLC1s, MyLC1f, MyLC2s and MyLC2f to actin content ratios remained unchanged. Hence, the underlying mechanisms in VIDD remain undefined and may arise from other factors than altered contents of, e.g. myosin and actin. This is consistent with the slow turnover rates of these proteins with half-lives of 5 days or longer [19, 42]. Post-translational modifications, including oxidation [43], on the other hand, offer alternative mechanisms underlying the modified propagation of the Ca2+ signal from the thin filament proteins to the cross-bridges in VIDD. Skeletal muscle is particularly vulnerable to oxidative stress. Six hours of mechanical ventilation promotes oxidative injury in the diaphragm, as indicated by the large increase in carbonyl derivatives [43]. It notably results in oxidation of myofibrillar proteins at molecular masses of 200 (MyHC) and 40 kDa (actin), altering their function [43].
In VIDD, other thin filament proteins may also be affected as indicated by the greater Hill coefficient (nH) of force and stiffness in type I fibres from piglets that were mechanically ventilated for 5 days compared with control animals. That is, the increase in nH and decrease in pCa50 may reflect a shift towards a faster troponin subunit isoform. The half-life of these particular proteins is approximately 4 days [19, 42]; a slow-to-fast isoform transformation cannot be excluded as previously shown during unloading [23]. In the present study, despite the use of sensitive silver-stained SDS-PAGE gels, we were not able to clearly identify and quantify the different troponin isoforms in single cells.
It appears unlikely that the anaesthetic agents used in the present experiment enhance the muscle fibre dysfunction considering that isoflurane and other intravenous anaesthetics such as ketamine, midazolam, propofol and thiopental have no direct effects on diaphragm contractility [2, 24].
EMD 57033-related changes
Seeking therapeutic strategies to minimise VIDD and Ca2+ desensitisation is clinically relevant. Ca2+ sensitisers, including EMD 57033, have been developed in attempts to solve similar problems in cardiac muscle [3, 12]. EMD 57033 is a prototype Ca2+ sensitiser. Based on solution studies, its main mechanism of action consists of Ca2+ sensitisation of some of the contractile proteins, i.e. thin filament proteins. This is mediated through Ca2+-dependent binding of the pharmacological agent to the Ca2+ subunit of the troponin complex, troponin C, more precisely to its slow skeletal/cardiac isoform, stabilising the Ca2+-induced conformation of the contractile proteins. EMD 57033 binds directly to the C-terminal region of troponin C, thereby affecting troponin C interaction with the inhibitory subunit of the troponin complex, troponin I [17, 41]. This displaces troponin I from actin towards troponin C, inducing the first tropomyosin movement towards the inner domain of actin. This will initiate an improved cross-bridge recruitment, thereby changing cross-bridge transition rates [13, 18] and ultimately resulting in an increased force-generating capacity.
The leftward shift of pCa50 of force in type I fibres from mechanically ventilated and control piglets exposed to the EMD 57033 compound (Table 2) indicates a significant hypersensitisation of force production at each sub-maximal Ca2+ concentration, i.e. less Ca2+ was needed to activate the diaphragm muscle fibres. To evaluate whether this effect was caused by an alteration in the number of strongly attached cross-bridges, the relative stiffness–pCa relationship was assessed. The higher pCa50 of stiffness in type I fibres from piglets belonging to MV and CTL groups following exposure to EMD 57033 (Table 2) demonstrates an enhanced relative number of recruited cross-bridges at the different Ca2+ concentrations. In spite of the unspecific inotropic effect of EMD 57033 on type I fibres from both mechanically ventilated and control piglets, it may nevertheless have a beneficial impact on diaphragm muscle function in VIDD. Similar beneficial action of another Ca2+ sensitiser, i.e. levosimendan, was recently reported in diaphragm muscle cells expressing the type I MyHC isoform from patients with chronic obstructive pulmonary disease [37].
The enhanced Ca2+ activation of contraction induced by EMD 57033 in type IIa fibres from control animals was an unexpected finding, especially since EMD 57033 has not been shown to bind to the fast skeletal troponin C isoform. However, the co-expression of slow skeletal/cardiac and fast skeletal troponin C isoforms [23] may offer an explanation to this result. The difference between type IIa control fibres and cells from mechanically ventilated animals may be secondary to a slow-to-fast troponin C isoform transition, i.e. a decrease in the expression of slow skeletal/cardiac troponin C isoform in favour of fast troponin C isoform in type IIa fibres, during mechanical ventilation as previously shown during unloading [23].
Clinical repercussions
Even though weaning failure in critically ill mechanically ventilated patients arises from multiple factors, including residual effects of sedative agents (e.g. hypnotics in combination with analgetics), abnormalities in lung mechanics, impaired oxygen delivery to muscles and psychological problems, VIDD appears to play a key role [11]. EMD 57033 partially counterbalances VIDD by restoring the force-generating capacity, especially at sub-maximal Ca2+ concentrations. Under in vivo conditions, diaphragm muscle does not generate maximum force, but shortens against sub-maximal loads, and the observed in vitro effects of EMD 57033 present significant potential therapeutic advantages [3, 12] such as (a) improvement of the effectiveness without increasing energy consumption during basal metabolism, excitation–contraction coupling and force generation and (b) no change in intracellular Ca2+ concentration, reducing the risk of Ca2+ overload.
Conclusions
Alterations in Ca2+ sensitivities of force and stiffness were observed in diaphragm muscle fibres from mechanically ventilated piglets compared with sham-operated animals, suggesting a less efficient Ca2+ activation of cross-bridges and subsequent force production. To further assess whether the impaired Ca2+ activation is reversible, the fibres were exposed to a Ca2+ sensitiser. The present results show that the addition of EMD 57033 partially restored the Ca2+ activation, indicating that treatment with Ca2+ sensitisers may provide an efficient therapeutic strategy in reducing VIDD.
References
Barclay CJ, Woledge RC, Curtin NA (2007) Energy turnover for Ca2+ cycling in skeletal muscle. J Muscle Res Cell Motil 28:259–274
Bouhemad B, Langeron O, Orliaguet G, Coriat P, Riou B (2002) Effects of halothane and isoflurane on the contraction, relaxation and energetics of rat diaphragmatic muscle. Br J Anaesth 89:479–485
Endoh M (2008) Cardiac ca(2+) signaling and ca(2+) sensitizers. Circ J 72:1915–1925
Esteban A, Anzueto A, Alia I, Gordo F, Apezteguia C, Palizas F, Cide D, Goldwaser R, Soto L, Bugedo G, Rodrigo C, Pimentel J, Raimondi G, Tobin MJ (2000) How is mechanical ventilation employed in the intensive care unit? An international utilization review. Am J Respir Crit Care Med 161:1450–1458
Esteban A, Frutos F, Tobin MJ, Alia I, Solsona JF, Valverdu I, Fernandez R, de la Cal MA, Benito S, Tomas R et al (1995) A comparison of four methods of weaning patients from mechanical ventilation. Spanish Lung Failure Collaborative Group. N Engl J Med 332:345–350
Fabiato A (1988) Computer programs for calculating total from specified free or free from specified total ionic concentrations in aqueous solutions containing multiple metals and ligands. Methods Enzymol 157:378–417
Frontera WR, Larsson L (1997) Contractile studies of single human skeletal muscle fibers: a comparison of different muscles, permeabilization procedures, and storage techniques. Muscle Nerve 20:948–952
Galler S, Hilber K (1998) Tension/stiffness ratio of skinned rat skeletal muscle fibre types at various temperatures. Acta Physiol Scand 162:119–126
Higuchi H, Yanagida T, Goldman YE (1995) Compliance of thin filaments in skinned fibers of rabbit skeletal muscle. Biophys J 69:1000–1010
Huxley AF (1971) The activation of striated muscle and its mechanical response. Proc R Soc Lond B Biol Sci 178:1–27
Jubran A (2006) Critical illness and mechanical ventilation: effects on the diaphragm. Respir Care 51:1054–1061 discussion 1062-1054
Kass DA, Solaro RJ (2006) Mechanisms and use of calcium-sensitizing agents in the failing heart. Circulation 113:305–315
Kraft T, Brenner B (1997) Force enhancement without changes in cross-bridge turnover kinetics: the effect of EMD 57033. Biophys J 72:272–281
Lamb GD, Posterino GS (2003) Effects of oxidation and reduction on contractile function in skeletal muscle fibres of the rat. J Physiol 546:149–163
Larsson L, Moss RL (1993) Maximum velocity of shortening in relation to myosin isoform composition in single fibres from human skeletal muscles. J Physiol 472:595–614
Levine S, Nguyen T, Taylor N, Friscia ME, Budak MT, Rothenberg P, Zhu J, Sachdeva R, Sonnad S, Kaiser LR, Rubinstein NA, Powers SK, Shrager JB (2008) Rapid disuse atrophy of diaphragm fibers in mechanically ventilated humans. N Engl J Med 358:1327–1335
Li MX, Spyracopoulos L, Beier N, Putkey JA, Sykes BD (2000) Interaction of cardiac troponin C with Ca(2+) sensitizer EMD 57033 and cardiac troponin I inhibitory peptide. Biochemistry 39:8782–8790
Lipscomb S, Preston LC, Robinson P, Redwood CS, Mulligan IP, Ashley CC (2005) Effects of troponin C isoform on the action of the cardiotonic agent EMD 57033. Biochem J 388:905–912
Martin AF (1981) Turnover of cardiac troponin subunits. Kinetic evidence for a precursor pool of troponin-I. J Biol Chem 256:964–968
Martyn DA, Smith L, Kreutziger KL, Xu S, Yu LC, Regnier M (2007) The effects of force inhibition by sodium vanadate on cross-bridge binding, force redevelopment, and Ca2+ activation in cardiac muscle. Biophys J 92:4379–4390
McDonald KS, Fitts RH (1995) Effect of hindlimb unloading on rat soleus fiber force, stiffness, and calcium sensitivity. J Appl Physiol 79:1796–1802
Moss RL (1979) Sarcomere length-tension relations of frog skinned muscle fibres during calcium activation at short lengths. J Physiol 292:177–192
Mounier Y, Tiffreau V, Montel V, Bastide B, Stevens L (2009) Phenotypical transitions and Ca2+ activation properties in human muscle fibers: effects of a 60-day bed rest and countermeasures. J Appl Physiol 106:1086–1099
Nishina K, Mikawa K, Kodama S, Kagawa T, Uesugi T, Obara H (2003) The effects of enflurane, isoflurane, and intravenous anesthetics on rat diaphragmatic function and fatigability. Anesth Analg 96:1674–1678 table of contents
Norman H, Kandala K, Kolluri R, Zackrisson H, Nordquist J, Walther S, Eriksson LI, Larsson L (2006) A porcine model of acute quadriplegic myopathy: a feasibility study. Acta Anaesthesiol Scand 50:1058–1067
Ochala J, Larsson L (2008) Effects of a preferential myosin loss on Ca2+ activation of force generation in single human skeletal muscle fibres. Exp Physiol 93:486–495
Ochala J, Li M, Ohlsson M, Oldfors A, Larsson L (2008) Defective regulation of contractile function in muscle fibres carrying an E41K beta-tropomyosin mutation. J Physiol 586:2993–3004
Powers SK, Kavazis AN, McClung JM (2007) Oxidative stress and disuse muscle atrophy. J Appl Physiol 102:2389–2397
Powers SK, Shanely RA, Coombes JS, Koesterer TJ, McKenzie M, Van Gammeren D, Cicale M, Dodd SL (2002) Mechanical ventilation results in progressive contractile dysfunction in the diaphragm. J Appl Physiol 92:1851–1858
Regnier M, Martin H, Barsotti RJ, Rivera AJ, Martyn DA, Clemmens E (2004) Cross-bridge versus thin filament contributions to the level and rate of force development in cardiac muscle. Biophys J 87:1815–1824
Sassoon CS, Zhu E, Caiozzo VJ (2004) Assist-control mechanical ventilation attenuates ventilator-induced diaphragmatic dysfunction. Am J Respir Crit Care Med 170:626–632
Seow CY, Shroff SG, Ford LE (1997) Detachment of low-force bridges contributes to the rapid tension transients of skinned rabbit skeletal muscle fibres. J Physiol 501(Pt 1):149–164
Shanely RA, Van Gammeren D, Deruisseau KC, Zergeroglu AM, McKenzie MJ, Yarasheski KE, Powers SK (2004) Mechanical ventilation depresses protein synthesis in the rat diaphragm. Am J Respir Crit Care Med 170:994–999
Shanely RA, Zergeroglu MA, Lennon SL, Sugiura T, Yimlamai T, Enns D, Belcastro A, Powers SK (2002) Mechanical ventilation-induced diaphragmatic atrophy is associated with oxidative injury and increased proteolytic activity. Am J Respir Crit Care Med 166:1369–1374
Solaro RJ, Gambassi G, Warshaw DM, Keller MR, Spurgeon HA, Beier N, Lakatta EG (1993) Stereoselective actions of thiadiazinones on canine cardiac myocytes and myofilaments. Circ Res 73:981–990
Spencer T, Posterino GS (2009) Sequential effects of GSNO and H2O2 on the Ca2+ sensitivity of the contractile apparatus of fast- and slow-twitch skeletal muscle fibers from the rat. Am J Physiol, Cell Physiol 296:C1015–C1023
van Hees HW, Dekhuijzen PN, Heunks LM (2009) Levosimendan enhances force generation of diaphragm muscle from patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med 179:41–47
Vannier C, Lakomkine V, Vassort G (1997) Tension response of the cardiotonic agent (+)-EMD-57033 at the single cell level. Am J Physiol 272:C1586–C1593
Vassilakopoulos T, Petrof BJ (2004) Ventilator-induced diaphragmatic dysfunction. Am J Respir Crit Care Med 169:336–341
Vassilakopoulos T, Zakynthinos S, Roussos C (1996) Respiratory muscles and weaning failure. Eur Respir J 9:2383–2400
Wang X, Li MX, Spyracopoulos L, Beier N, Chandra M, Solaro RJ, Sykes BD (2001) Structure of the C-domain of human cardiac troponin C in complex with the Ca2+ sensitizing drug EMD 57033. J Biol Chem 276:25456–25466
Zak R, Martin AF, Blough R (1979) Assessment of protein turnover by use of radioisotopic tracers. Physiol Rev 59:407–447
Zergeroglu MA, McKenzie MJ, Shanely RA, Van Gammeren D, DeRuisseau KC, Powers SK (2003) Mechanical ventilation-induced oxidative stress in the diaphragm. J Appl Physiol 95:1116–1124
Acknowledgements
This study was supported by grants from the Swedish Institute and Association Française contre les Myopathies to J.O. and from the Swedish Research Council (08651), Association Française contre les Myopathies, Cancer Foundation and National Institutes of Health (AR045627, AR047318) to L.L. EMD 57033 was a gift from Dr. Norbert Beier from Merck KGaA, Darmstadt, Germany. We are grateful to Yvette Hedström and Ann-Marie Gustafsson for excellent technical assistance.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ochala, J., Radell, P.J., Eriksson, L.I. et al. EMD 57033 partially reverses ventilator-induced diaphragm muscle fibre calcium desensitisation. Pflugers Arch - Eur J Physiol 459, 475–483 (2010). https://doi.org/10.1007/s00424-009-0744-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00424-009-0744-1