Abstract
Purpose
In a recent meta-analysis of 38 double-blind randomized controlled trials (RCTs) comparing pregabalin (PGB) to placebo, we found 20 adverse events (AEs) to be significantly associated with PGB treatment. In the present study, we evaluated whether the incidence of these 20 AEs differs across distinct disorders in which PGB was investigated.
Methods
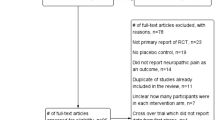
Among the 38 previously identified RCTs of PGB, we selected only those including a PGB 600 mg/day arm and subsequently classified them into four distinct groups according to the disorder in which PGB was investigated: (1) drug-resistant partial epilepsy, (2) psychiatric disorders, (3) fibromyalgia, and (4) neuropathic pain. We used risk differences (RDs) to quantify the placebo-corrected proportion of subjects discontinuing PGB due to intolerable AEs and to determine the placebo-corrected incidence of each of the 20 PGB AEs across the four disorders.
Results
Twenty-two RCTs were included in this study. Neither the proportion of subjects discontinuing PGB due to intolerable AEs nor the incidence of PGB AEs (with the exception of ataxia) differed significantly across the four disorders. Ataxia was more common in drug-resistant partial epilepsy compared to fibromyalgia. When limiting analyses to subjects on placebo, most vestibulo-cerebellar AEs (ataxia, diplopia, and blurred vision) were found to be more common in drug-resistant partial epilepsy compared to all other disorders. Diplopia and blurred vision were more common in epilepsy than in neuropathic pain; and ataxia had a higher incidence in epilepsy than in anxiety disorder and fibromyalgia. Among other CNS AEs, somnolence was more common in epilepsy compared to neuropathic pain and in anxiety disorders alone compared to neuropathic pain and fibromyalgia. Asthenia was also more common in epilepsy than in neuropathic pain and fibromyalgia.
Conclusions
Although drug-resistant partial epilepsy is associated with a higher probability of developing vestibulo-cerebellar AEs, the risk for PGB toxicity does not differ across distinct disorders.


Similar content being viewed by others
References
Marson AG, Kadir ZA, Hutton JL, Chadwick DW (1997) The new antiepileptic drugs: a systematic review of their efficacy and tolerability. Epilepsia 38:859–880
Marson AG, Kadir ZA, Hutton JL, Chadwick DW (2000) Gabapentin for drug-resistant partial epilepsy. Cochrane Database Syst Rev (2): CD001415. Update in: Cochran Database Syst Rev 2000;3: CD001415
Chadwick DW, Marson AG (2000) Zonisamide for drug-resistant partial epilepsy. Cochrane Database Syst Rev (2):CD001416. Update in: Cochrane Database Syst Rev 2002;2:CD001416
Jette NJ, Marson AG, Kadir ZA, Hutton JL (2000) Topiramate for drugresistant partial epilepsy. Cochrane Database Syst Rev (2):CD001417. Update in: Cochran Database Syst Rev 2002;3:CD001417
Ramaratnam S, Marson AG, Baker GA (2001) Lamotrigine add-on for drug-resistant partial epilepsy. Cochrane Database Syst Rev 2000; (3):CD001909. Update in: Cochrane Database Syst Rev 3:CD001909
Chaisewikul R, Privitera MD, Hutton JL, Marson AG (2001) Levetiracetam add-on for drug-resistant localization related (partial) epilepsy. Cochrane Database Syst Rev (1):CD001901
Marson AG, Hutton JL, Leach JP, Castillo S, Schmidt D, White S, Chaisewikul R, Privitera M, Chadwick DW (2001) Levetiracetam, oxcarbazepine, remacemide and zonisamide for drug resistant localization-related epilepsy: a systematic review. Epilepsy Res 46:259–270
Chadwick DW, Marson AG (2002) Zonisamide add-on for drug-resistant partial epilepsy. Cochrane Database Syst Rev (4):CD001416. Update in: Cochran Database Syst Rev 2005;4:CD001416.
Leach JP, Marson AG, Hutton JL (2002) Remacemide for drug-resistant localization related epilepsy. Cochrane Database Syst Rev 4:CD001900
Pereira J, Marson AG, Hutton JL (2002) Tiagabine add-on for drug-resistant partial epilepsy. Cochrane Database Syst Rev (3):CD001908
Chadwick DW, Marson AG (2005) Zonisamide add-on for drug-resistant partial epilepsy. Cochrane Database Syst Rev (4):CD001416
Hemming K, Maguire MJ, Hutton JL, Marson AG (2008) Vigabatrin for refractory partial epilepsy. Cochrane Database Syst Rev 2008; (3):CD007302
Jette N, Hemming K, Hutton JL, Marson AG (2008) Topiramate add-on for drug-resistant partial epilepsy. Cochrane Database Syst Rev (3):CD001417
Lozsadi D, Hemming K, Marson AG (2008) Pregabalin add-on for drug resistant partial epilepsy. Cochrane Database Syst Rev (1):CD005612
Michael B, Marson AG (2008) Clobazam as an add-on in the management of refractory epilepsy. Cochrane Database Syst Rev (2):CD004154
Zaccara G, Gangemi PF, Perucca P, Specchio L (2011) The adverse event profile of pregabalin: A systematic review and meta-analysis of randomized controlled trials. Epilepsia (in print). doi:10.1111/j.1528-1167.2010.02966.x
Higgins JPT, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. Br Med J 327:557–560
RevMan (2008) Review Manager (RevMan) [computer program]. Version 5.1. The Nordic Cochrane Centre, The Cochrane Collaboration, Copenhagen
Fleiss JL (1981) Statistical methods for rates and proportions. Wiley, New York, pp 13–17
Arroyo S, Anhut H, Kugler AR, Lee CM, Knapp LE, Garofalo EA, Messmer S (2004) Pregabalin add-on treatment: a randomized, double-blind, placebo-controlled, dose-response study in adults with partial seizures. Epilepsia 45(1):20–27
Beydoun A, Uthman BM, Kugler AR, Greiner MJ, Knapp LE, Garofalo EA, Pregabalin 1008-009 Study Group (2005) Safety and efficacy of two pregabalin regimens for add-on treatment of partial epilepsy. Neurology 64(3):475–480
Elger CE, Brodie MJ, Anhut H, Lee CM, Barrett JA (2005) Pregabalin add-on treatment in patients with partial seizures: a novel evaluation of flexible-dose and fixed-dose treatment in a double-blind, placebo-controlled study. Epilepsia 46(12):1926–1936
French JA, Kugler AR, Robbins JL, Knapp LE, Garofalo EA (2003) Dose-response trial of pregabalin adjunctive therapy in patients with partial seizures. Neurology 60(10):1631–1637
Feltner DE, Crockatt JG, Dubovsky SJ, Cohn CK, Shrivastava RK, Targum SD, Liu-Dumaw M, Carter CM, Pande AC (2003) A randomized, double-blind, placebo-controlled, fixed-dose, multicenter study of pregabalin in patients with generalized anxiety disorder. J Clin Psychopharmacol 23(3):240–249
Montgomery SA, Tobias K, Zornberg GL, Kasper S, Pande AC (2006) Efficacy and safety of pregabalin in the treatment of generalized anxiety disorder: a 6-week, multicenter, randomized, double-blind, placebo-controlled comparison of pregabalin and venlafaxine. J Clin Psychiatry 67(5):771–782
Pande AC, Crockatt JG, Feltner DE, Janney CA, Smith WT, Weisler R, Londborg PD, Bielski RJ, Zimbroff DL, Davidson JR, Liu-Dumaw M (2003) Pregabalin in generalized anxiety disorder: a placebo-controlled trial. Am J Psychiatry 160(3):533–540
Pande AC, Feltner DE, Jefferson JW, Davidson JR, Pollack M, Stein MB, Lydiard RB, Futterer R, Robinson P, Slomkowski M, DuBoff E, Phelps M, Janney CA, Werth JL (2004) Efficacy of the novel anxiolytic pregabalin in social anxiety disorder: a placebo-controlled, multicenter study. J Clin Psychopharmacol 24(2):141–149
Rickels K, Pollack MH, Feltner DE, Lydiard RB, Zimbroff DL, Bielski RJ, Tobias K, Brock JD, Zornberg GL, Pande AC (2005) Pregabalin for treatment of generalized anxiety disorder: a 4-week, multicenter, double-blind, placebo-controlled trial of pregabalin and alprazolam. Arch Gen Psychiatry 62(9):1022–1030
Arnold LM, Russell IJ, Diri EW, Duan WR, Young JP Jr, Sharma U, Martin SA, Barrett JA, Haig G (2008) A 14-week, randomized, double-blinded, placebo-controlled monotherapy trial of pregabalin in patients with fibromyalgia. J Pain 9(9):792–805
Mease PJ, Russell IJ, Arnold LM, Florian H, Young JP Jr, Martin SA, Sharma U (2008) A randomized, double-blind, placebo-controlled, phase III trial of pregabalin in the treatment of patients with fibromyalgia. J Rheumatol 35(3):502–514
Anonymous (2008) A 14 week, randomized, double-blind, placebo-controlled trial of pregabalin twice daily in patients with fibromyalgia. Protocol no. A0081100, clinical study synopsis
Arezzo JC, Rosenstock J, Lamoreaux L, Pauer L (2008) Efficacy and safety of pregabalin 600 mg/d for treating painful diabetic peripheral neuropathy: a double-blind placebo-controlled trial. BMC Neurol 16(8):33
Lesser H, Sharma U, LaMoreaux L, Poole RM (2004 ) Pregabalin relieves symptoms of painful diabetic neuropathy: a randomized controlled trial. Neurology 63(11):2104–2110
Richter RW, Portenoy R, Sharma U, Lamoreaux L, Bockbrader H, Knapp LE (2005) Relief of painful diabetic peripheral neuropathy with pregabalin: a randomized, placebo-controlled trial. J Pain 6(4):253–260
Tölle T, Freynhagen R, Versavel M, Trostmann U, Young JP Jr (2008) Pregabalin for relief of neuropathic pain associated with diabetic neuropathy: a randomized, double-blind study. Eur J Pain 12(2):203–213
Anonymous (2007) A placebo-controlled trial of pregabalin and amitriptyline for treatment of painful diabetic peripheral neuropathy. Protocol no. 1008-040, PhRMA clinical study dynopsis
Anonymous (2007) A randomized, double-blind, placebo-controlled, parallel-group, multi-center trial of pregabalin versus placebo in the treatment of neuropathic pain associated with diabetic peripheral neuropathy. Protocol no. A0081071, clinical study synopsis
Freynhagen R, Strojek K, Griesing T, Whalen E, Balkenohl M (2005) Efficacy of pregabalin in neuropathic pain evaluated in a 12-week, randomised, double-blind, multicentre, placebo-controlled trial of flexible- and fixed-dose regimens. Pain 115(3):254–263
Anonymous (2009) A 13-week, randomized, double-blind, multicenter, placebo-controlled study toevaluate efficacy and safety of pregabalin (CI-1008) in the treatment of postherpetic neuralgia. Protocol no. A0081120, clinical study synopsis
Dworkin RH, Corbin AE, Young JP Jr, Sharma U, LaMoreaux L, Bockbrader H, Garofalo EA, Poole RM (2003) Pregabalin for the treatment of postherpetic neuralgia: a randomized, placebo-controlled trial. Neurology 60(8):1274–1283
van Seventer R, Feister HA, Young JP Jr, Stoker M, Versavel M, Rigaudy L (2006) Efficacy and tolerability of twice-daily pregabalin for treating pain and related sleep interference in postherpetic neuralgia: a 13-week, randomized trial. Curr Med Res Opin 22(2):375–384
Sirven JI, Fife TD, Wingerchuk DM, Drazkowski JF (2007) Second-generation antiepileptic drugs' impact on balance: a meta-analysis. Mayo Clin Proc 82:40–47
Hoppener RJ, Kuyer A, Meijer JWA, Hulsman J (1980) Correlation between daily fluctuations of carbamazepine serum levels and intermittent side effects. Epilepsia 21:341–350
Zaccara G, Cincotta M, Borgheresi A, Balestrieri F (2004) Adverse motor effects induced by antiepileptic drugs. Epileptic Disord 6:153–168
Berg AT (2011) Epilepsy, cognition, and behavior: the clinical picture. Epilepsia 52(Suppl 1):7–12
Malow BA (2007) The interaction between sleep and epilepsy. Epilepsia 48(Suppl 9):36–38
Ietsugu T, Sukigara M, Furukawa TA (2007) Evaluation of diagnostic criteria for panic attack using item response theory: findings from the National Comorbidity Survey in USA. J Affect Disord 104:197–201
Civeira F, Basallo F (1970) The diabetic heart. Diabete 18:166–170
Barsky AJ, Saintfort R, Rogers MP, Borus JF (2002) Nonspecific medication side effects and the nocebo phenomenon. JAMA 287:622–627
Enck P, Benedetti F, Schedlowski M (2008) New insights into the placebo and nocebo responses. Neuron 59:195–206
Amanzio M, Corazzini LL, Vase L, Benedetti F (2009) A systematic review of adverse events in placebo groups of anti-migraine clinical trials. Pain 146:261–269
Papadopoulos D, Mitsikostas DD (2010) Nocebo effects in multiple sclerosis trials: a meta-analysis. Mult Scler 16:816–828
Acknowledgments
We are grateful to Ettore Beghi for his valuable comments.
Funding
The authors received no funding for this study.
Disclosure
G.Z. has received speaker’s or consultancy fees from EISAI, Jansen-Cilag, Novartis, Sanofi-Aventis, and UCB Pharma. P.P. is the recipient of the Susan S. Spencer Clinical Research Training Fellowship in Epilepsy supported by the American Academy of Neurology Foundation, the American Epilepsy Society, and the Epilepsy Foundation. P.G. reports no disclosures.
Author information
Authors and Affiliations
Corresponding author
Appendices
Appendix 1
Table 2 compares the placebo-corrected incidence of PGB AEs across four distinct disorders.
Appendix 2
Table 3 presents the incidence of adverse events (AEs) in subjects taking placebo across four distinct disorders.
Rights and permissions
About this article
Cite this article
Zaccara, G., Perucca, P. & Gangemi, P.F. The adverse event profile of pregabalin across different disorders: a meta-analysis. Eur J Clin Pharmacol 68, 903–912 (2012). https://doi.org/10.1007/s00228-012-1213-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-012-1213-x