Abstract
Purpose
Our aim was to study drug interactions and dose adjustments in patients with renal impairment in the discharge medication of surgical inpatients and to evaluate the strengths and limitations of clinical decision support software (CDSS) for this task.
Methods
This was a cross-sectional study involving 509 surgical patients of a primary care hospital. We developed a customized interface for the CDSS MediQ, which we used for automated retrospective identification of drug interactions in the patients’ discharge medication. The clinical relevance of the interactions was evaluated based on the Zurich Interaction System (ZHIAS) that incorporates the operational classification of drug interactions (ORCA). Prescriptions were further analyzed for recommended dose adjustments in patients with a glomerular filtration rate <60 ml/min.
Results
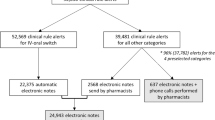
For the total of 2,729 prescriptions written for the 509 patients enrolled in the study, MediQ generated 2,558 interaction alerts and 1,849 comments. Among these were ten “high danger” and 551 “average danger” alerts that we reclassified according to ORCA criteria. This reclassification resulted in ten contraindicated combinations, 77 provisionally contraindicated combinations, and 310 with a conditional and 164 with a minimal risk of adverse outcomes. The ZHIAS classification also provides categorical information on expected adverse outcomes and management recommendations, which are presented in detail. We identified 56 prescriptions without a recommended dose adjustment for impaired renal function.
Conclusions
CDSS identified a large number of drug interactions in surgical discharge medication, but according to ZHIAS criteria only a minor fraction of these appeared to involve a substantial risk to the patient. CDSS should therefore aim at reducing over-alerting and improve usability in order to become more efficacious in terms of the prevention of adverse drug events in clinical practice.


Similar content being viewed by others
References
Bates DW, Cullen DJ, Laird N, Petersen LA, Small SD, Servi D, Laffel G, Sweitzer BJ, Shea BF, Hallisey R et al (1995) Incidence of adverse drug events and potential adverse drug events. Implications for prevention. ADE Prevention Study Group. JAMA 274(1):29–34
Classen DC, Pestotnik SL, Evans RS, Lloyd JF, Burke JP (1997) Adverse drug events in hospitalized patients. Excess length of stay, extra costs, and attributable mortality. JAMA 277(4):301–306
Lazarou J, Pomeranz BH, Corey PN (1998) Incidence of adverse drug reactions in hospitalized patients: a meta-analysis of prospective studies. JAMA 279(15):1200–1205
Pirmohamed M, James S, Meakin S, Green C, Scott AK, Walley TJ, Farrar K, Park BK, Breckenridge AM (2004) Adverse drug reactions as cause of admission to hospital: prospective analysis of 18 820 patients. Br Med J 329(7456):15–19
Vonbach P, Dubied A, Beer JH, Krähenbühl S (2007) Recognition and management of potential drug–drug interactions in patients on internal medicine wards. Eur J Clin Pharmacol 63(11):1075–1083
Kaushal R, Shojania KG, Bates DW (2003) Effects of computerized physician order entry and clinical decision support systems on medication safety: a systematic review. Arch Intern Med 163(12):1409–1416
Raschke RA, Gollihare B, Wunderlich TA, Guidry JR, Leibowitz AI, Peirce JC, Lemelson L, Heisler MA, Susong C (1998) A computer alert system to prevent injury from adverse drug events: development and evaluation in a community teaching hospital. JAMA 280(15):1317–1320
Bates DW, Teich JM, Lee J, Seger D, Kuperman GJ, Ma'Luf N, Boyle D, Leape L (1999) The impact of computerized physician order entry on medication error prevention. J Am Med Inform Assoc 6(4):313–321
Lin CP, Payne TH, Nichol WP, Hoey PJ, Anderson CL, Gennari JH (2008) Evaluating clinical decision support systems: monitoring CPOE order check override rates in the Department of Veterans Affairs' Computerized Patient Record System. J Am Med Inform Assoc 15(5):620–626
van der Sijs H, Aarts J, Vulto A, Berg M (2006) Overriding of drug safety alerts in computerized physician order entry. J Am Med Inform Assoc 13(2):138–147
Weingart SN, Toth M, Sands DZ, Aronson MD, Davis RB, Phillips RS (2003) Physicians' decisions to override computerized drug alerts in primary care. Arch Intern Med 163(21):2625–2631
Taylor LK, Tamblyn R (2004) Reasons for physician non-adherence to electronic drug alerts. Stud Health Technol Inform 107(Pt 2):1101–1105
Lin J, Knight EL, Hogan ML, Singh AK (2003) A comparison of prediction equations for estimating glomerular filtration rate in adults without kidney disease. J Am Soc Nephrol 14(10):2573–2580
Aronoff GR, Bennett WM, Berns JS (2007) Drug prescribing in renal failure: dosing guidelines for adults and children. American College of Physicians, Philadelphia
Hansten PD, Horn JR, Hazlet TK (2001) ORCA: OpeRational ClassificAtion of drug interactions. J Am Pharm Assoc (Wash) 41(2):161–165
Hansten PD, Horn JR (2010) Drug interactions: analysis and management. Wolters Kluwer Health, St. Louis
Baxter K, Stockley IH (2010) Stockley's drug interactions : a source book of interactions, their mechanisms, clinical importance, and management. Pharmaceutical Press, London/Chicago
Malone DC, Abarca J, Hansten PD, Grizzle AJ, Armstrong EP, Van Bergen RC, Duncan-Edgar BS, Solomon SL, Lipton RB (2004) Identification of serious drug-drug interactions: results of the partnership to prevent drug-drug interactions. J Am Pharm Assoc 44(2):142–151
Hinz B, Cheremina O, Bachmakov J, Renner B, Zolk O, Fromm MF, Brune K (2007) Dipyrone elicits substantial inhibition of peripheral cyclooxygenases in humans: new insights into the pharmacology of an old analgesic. FASEB J 21(10):2343–2351
Graff J, Arabmotlagh M, Cheung R, Geisslinger G, Harder S (2007) Effects of parecoxib and dipyrone on platelet aggregation in patients undergoing meniscectomy: a double-blind, randomized, parallel-group study. Clin Ther 29(3):438–447
Acknowledgments
The authors would like to thank the Information Technology Department at the General Hospital Männedorf for providing files on the source population.
Financial support and conflict of interest statement
This study was financed by internal resources from the Department of Clinical Pharmacology. The manuscript was made available to Eveline Jaquenoud Sirot, MediQ, Aargau, Switzerland, before submission, but MediQ had no influence on the study design, analysis, or interpretation of the results.
All authors declare that they have no conflict of interest in relation to the presented study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Frölich, T., Zorina, O., Fontana, A.O. et al. Evaluation of medication safety in the discharge medication of 509 surgical inpatients using electronic prescription support software and an extended operational interaction classification. Eur J Clin Pharmacol 67, 1273–1282 (2011). https://doi.org/10.1007/s00228-011-1081-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-011-1081-9