Abstract
Objective
To evaluate the concentration of metronidazole in muscle tissue using microdialysis and to compare it with plasma concentration and in vitro-defined MIC90 (minimal inhibiting concentration) for the most frequent anaerobic bacteria isolated in our hospital.
Materials and methods
Six female patients scheduled for elective gynaecological surgery were included. Exclusion criteria were active inflammatory process and being overweight (BMI more than 30). Microdialysis catheters (CMA 60 catheters with 20 kDa cut-off membrane) were placed into the m. vastus lateralis. The microdialysis perfusion rate was 2 μl/min. To assess in vivo recovery of the drug, retrodialysis with a 5-mg/l solution of metronidazole was performed. Microdialysis and blood samples were collected simultaneously 10 h after metronidazole administration. MIC90 data were obtained from the database of the microbiology laboratory of the local hospital.
Results
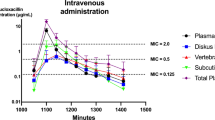
Data from five patients were included in analysis. The metronidazole concentration in blood achieved a value of 16.5±4.6 mg/l at 30 min (first available data), while in muscle a maximum level of 7.8±1.5 mg/l was achieved at 114 min. The mean MIC90 for the Bacteroides fragilis group was 0.25±0.26 mg/l. Data from mean plasma concentrations were fitted into the two-compartmental model and time over MIC90 and time over four times MIC90 were calculated, which were 52.1±13.5 h and 33.2±8.7 h, respectively. The Cmax/MIC90 ratio was 65.8±18.5 for plasma and 31.1±6.2 for muscle.
Conclusion
The present data demonstrate that metronidazole penetrates well into muscle tissue. Muscle tissue concentrations reach values far greater than MIC90 for the Bacteroides fragilis group and persist at such high levels for at least 10 h.

Similar content being viewed by others
References
Mittendorf R, Aronson MP, Berry RE et al (1993) Avoiding serious infections associated with abdominal hysterectomy: a meta-analysis of antibiotic prophylaxis. Am J Obstet Gynecol 169:1119–1124
Hardman JG, Limbird LE (1996) Goodman and Gilman’s The pharmacological basis of therapeutics. McGraw-Hill, New York
Müller M, Brunner M, Hollenstein U et al (1999) Penetration of ciprofloxacin into the interstitial of inflammed foot lesions in non-insulin-dependent diabetes mellitus patients Antimicrobial Agents Chemother 43:2056–2058
Joukhadar C, Frossard M, Mayer BX et al (2001) Impaired target site penetration of β-lactams may account for therapeutic failure in patients with septic shock. Crit Care Med 29:385–391
Brunner M, Pernerstorfer T, Mayer BX., Eichler HG, Müller M (2000) Surgery and intensive care procedures affect target site distribution of piperacillin. Crit Care Med 28:1754–1759
Hollenstein U, Brunner M, Mayer BX et al (2000) Target site concentrations after continuous infusion and bolus injection of cefpirome to healthy volunteers. Clin Pharmacol Ther 67:229–236
Müller M (2002) Microdialysis. Br Med J 324:588–591
Kling P, Burman LG (1989) Serum and tissue pharmacokinetics of intravenous metronidazole in surgical patients. Acta Chir Scand 155:347–350
Lamp K, Freeman CD, Klutman NE, Lacy MK (1999) Pharmacokinetics and pharmacodynamics of nitroimidazole antimicrobials. Clin Pharmacokinet 36:353–373
Lares-Asseff I, Cravioto J, Santiago P, Perez-Ortiz B (1992) Pharmacokinetics of metronidazole in severely malnourished and nutritionally rehabilitated children. Clin Pharmacol Ther 51:42–50
Klimowicz A, Nowak A, Bielecka-Grzela S (1996) Plasma and skin blister fluid concentration of metronidazole and its hydroxymetabolite after oral administration. Pol J Pharmacol 48:47–52
Kerin MJ, Greenstein D, Chisholm EM, Sheehan SJ, Kester RC (1992) Is antibiotic penetration compromised in the ischaemic tissues of patients undergoing amputation? Ann R Coll Surg Engl 74:274–276
Plaisance KI, Quintiliani R, Nightingale CH (1988) The pharmacokinetics of metronidazole and its metabolites in critically ill patients. J Antimicrob Chemother 21:195–200
Levy Y, Berger SA, Gorea A, Shnaker A, Orda R (1996) Penetration of clindamycin and metronidazole into inflammed appendicial tissue. Eur J Surg 162:633–635
Aitkenhead AR, Rowbotam DJ, Smith G (2001) Textbook of anaesthesia. Churchill Livingstone, Edinburgh
Ståhle L, Segersvärd S, Ungerstedt U (1991) A comparison between three methods for estimation of extracellular concentrations of exogenous and endogenous compounds by microdialysis. J Pharmacol Methods 25:41–52
Lõivukene K, Naaber P (2002) Antibiotic susceptibility of anaerobic bacteria in Estonia. In: Abstract book of the 6th Biennial Congress of the Anaerobe Society of the Americas. Utah, p 90
Hand WL, King-Thompson N, Holman JW (1987) Entry of roxithromycin (RU 965), imipenem, cefotaxime, trimethoprime, and metronidazole into human polymorphonuclear leukocytes. Antimicrobial Agents Chemother 31:1553–1557
Mandell GL, Douglas RG, Bennet JE (1990) Principles and practice of infectious diseases. Churchill Livingstone, New York
Bruegger D, Bauer A, Finsterer U, Bernasconi P, Kreimeier U, Christ F (2002) Microvascular changes during anesthesia: sevoflurane compared with propofol. Acta Anaesthesiol Scand 46:481–487
Acknowledgments
Authors are grateful to Professor Aleksander Zharkovski and Dr. Dmitri Avlassevitch for their valuable help in preparing this document. This work was supported by Estonian Science Foundation grants no. 5304 and no. 4428.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Karjagin, J., Pähkla, R. & Starkopf, J. Perioperative penetration of metronidazole into muscle tissue: a microdialysis study. Eur J Clin Pharmacol 59, 809–813 (2004). https://doi.org/10.1007/s00228-003-0685-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-003-0685-0