Abstract
Objective
Rapid functional recovery and improved range of motion after total knee arthroplasty (TKA) without compromising implant position.
Indications
Osteoarthritis of the knee requiring TKA.
Contraindications
Preoperative flexion < 80°.
Flexion contracture > 20°.
Body mass index > 40 kg/m2.
Fixed valgus deformity > 15°.
Relative: previous open surgery on the knee; systematic steroids (skin fragility); tall muscular males.
Surgical Technique
Straight skin incision over the medial third of the patella from 2 cm proximal to the patella, and then to the level of the tibial tuberosity. Extension of capsular incision 2 cm into the vastus medialis muscle from a point 2 cm proximal to the patella. Deep incision around the medial border of the patella and distally to the level of the tibial tuberosity. The patella is displaced laterally but is not everted in flexion. Knee flexion and extension as necessary to move the soft-tissue surgical window for proximal or distal exposure. Hyperflexion of the knee only for insertion of the tibial component.
Postoperative Management
Knee flexion exercises extension/flexion 0-0-70° using continuous passive motion the day after surgery. Weight bearing to tolerance allowed at 1st day after surgery (walker, two crutches). Thrombosis prophylaxis.
Results
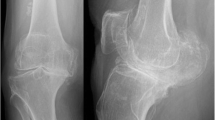
69 patients with 74 TKAs done through the mini-incision mid-vastus approach were available with a minimum 1-year follow-up. A control group was evaluated retrospectively including 52 patients with 57 total knee replacements in which a standard medial parapatellar arthrotomy with patella eversion was used. At all clinical evaluations flexion and the ability to climb stairs were significantly superior in the mid-vastus group indicating a faster recovery and return to functional activities. There were no complications and the radiographic evaluation found no implant or limb malalignment, or signs of early loosening.
Zusammenfassung
Operationsziel
Schnellere Wiederherstellung der Kniegelenkfunktion mit verbesserter Beweglichkeit nach Implantation einer Kniegelenkprothese mit sicherer Implantatpositionierung.
Indikationen
Implantation von Knieendoprothesen bei Gonarthrose.
Kontraindikationen
Präoperative Flexion < 80°.
Beugekontraktur > 20°.
Body-Mass-Index > 40 kg/m2.
Kontrakte Valgusdeformität > 15°.
Relativ: Vorherige Arthrotomie des Kniegelenks; systemische Steroideinnahme (Hautfragilität); grosse muskelstarke Männer.
Operationstechnik
Gerader Hautschnitt, über dem medialen Drittel der Patella beginnend, 2 cm proximal der Patella bis zur Tuberositas tibiae. Tiefe mediale parapatellare Inzision der Kapsel von der Tuberositas tibiae bis 2 cm proximal der oberen medialen „Patellaecke“, Erweiterung der Inzision über 2 cm im Faserverlauf des Musculus vastus medialis. Die Patella wird lateralisiert, aber nicht vollständig evertiert. Notwendigenfalls wird durch Beugung und Streckung des Gelenks das Weichteilfenster zur besseren Darstellung nach proximal und distal verlagert. Eine überspitzwinklige Beugung des Gelenks ist nur zur Einbringung der tibialen Komponente notwendig.
Weiterbehandlung
Krankengymnastische Übungsbehandlung mit CPM-(„continuous passive motion-)Schienen-Anwendung (Extension/Flexion 0-0-70°) und schmerzadaptierte Vollbelastung am 1. postoperativen Tag (Gehwagen, zwei Unterarmgehstützen). Thromboseprophylaxe.
Ergebnisse
Von 74 Kniegelenkprothesen (69 Patienten), die über einen Midvastus-Zugang mit verkürzter Muskelinzision implantiert wurden, wurde das Ergebnis nach mindestens 1 Jahr evaluiert und mit einer Kontrollgruppe verglichen (57 Kniegelenkprothesen, 52 Patienten), bei der eine mediale parapatellare Standardarthrotomie mit vollständiger Patellaeversion verwendet wurde. Die klinischen Ergebnisse der Midvastus-Gruppe bestätigten zu allen Untersuchungszeitpunkten eine signifikant bessere Flexion und Fähigkeit, Treppen zu steigen, was eine schnellere Wiederherstellung der Kniegelenkfunktion und Rückkehr zu funktionellen Aktivitäten bedeutet. Komplikationen traten nicht auf, und die radiologischen Untersuchungen zeigten keine Implantatfehllagen, keine Achsfehlstellungen oder Anzeichen für frühzeitige Implantatlockerungen.
Similar content being viewed by others
References
Bäthis H, Perlick L, Blum C, et al. Midvastus approach in total knee arthroplasty: a randomized, double-blinded study on early rehabilitation. Knee Surg Sports Traumatol Arthrosc 2005;13:545–550.
Berend KR, Lombardi AV Jr. Avoiding the potential pitfalls of minimally invasive total knee surgery. Orthopedics 2005;28:1326–1330.
Bonutti PM, Mont MA, Kester MA. Minimally invasive total knee arthroplasty: a 10-feature evolutionary approach. Orthop Clin North Am 2004;35:217–226.
Bonutti PM, Neal DJ, Kester MA. Minimal incision total knee arthroplasty using the suspended leg technique. Orthopedics 2003;26:899–903.
Buechel FF Sr. Long-term followup after mobile-bearing total knee replacement. Clin Orthop 2002;404:40–50.
Dalury DF, Dennis DA. Mini-incision total knee arthroplasty can increase risk of component malalignment. Clin Orthop 2005;440:77–81.
Dalury DF, Jiranek WA. A comparison of the midvastus and paramedian approaches for total knee arthroplasty. J Arthroplasty 1999;14:33–37.
Engh GA, Holt BT, Parks NL. A midvastus muscle-splitting approach for total knee arthroplasty. J Arthroplasty 1997;12:322–331.
Ewald FC. The Knee Society total knee arthroplasty roentgenographic evaluation and scoring system. Clin Orthop 1989;248:9–12.
Flören M, Davis J, Peterson MG, et al. A mini-midvastus capsular approach with patellar displacement decreases the prevalence of patella baja. J Arthroplasty 2007;22:Suppl 2:51–57.
Gregori A. Minimally invasive navigated knee surgery: a European perspective. Orthopedics 2005;28:Suppl:1235–1239.
Haas SB, Cook S, Beksac B. Minimally invasive total knee replacement through a mini midvastus approach: a comparative study. Clin Orthop 2004;428:68–73.
Hofmann AA, Plaster RL, Murdock LE. Subvastus (Southern) approach for primary total knee arthroplasty. Clin Orthop 1991;269:70–77.
Insall J. A midline approach to the knee. J Bone Joint Surg Am 1971;53:1584–1586.
Insall JN, Dorr LD, Scott RD, et al. Rationale of the Knee Society clinical rating system. Clin Orthop 1989;248:13–14.
Keating EM, Meding JB, Faris PM, et al. Long-term followup of nonmodular total knee replacements. Clin Orthop 2002;404:34–39.
Keblish PA. The lateral approach for total knee arthroplasty. J Knee Surg 2003;16:62–68.
Laskin RS, Beksac B, Phongjunakorn A, et al. Minimally invasive total knee replacement through a mini-midvastus incision: an outcome study. Clin Orthop 2004;428:74–81.
Maestro A, Suarez MA, Rodriguez L, et al. The midvastus surgical approach in total knee arthroplasty. Int Orthop 2000;24:104–107.
Ritter MA, Berend ME, Meding JB, et al. Long-term followup of anatomic graduated components posterior cruciate-retaining total knee replacement. Clin Orthop 2001;388:51–57.
Rodriguez JA, Bhende H, Ranawat CS. Total condylar knee replacement: a 20-year followup study. Clin Orthop 2001;388:10–17.
Tria AJ Jr, Coon TM. Minimal incision total knee arthroplasty: early experience. Clin Orthop 2003;416:185–190.
White RE Jr, Allman JK, Trauger JA, Dales BH. Clinical comparison of the midvastus and medial parapatellar surgical approaches. Clin Orthop 1999;367:117–122.
Worland RL, Johnson GV, Alemparte J, et al. Ten to fourteen year survival and functional analysis of the AGC total knee replacement system. Knee 2002;9:133–137.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Flören, M., Reichel, H., Davis, J. et al. The Mini-Incision Mid-Vastus Approach for Total Knee Arthroplasty. Orthop Traumatol 20, 534–543 (2008). https://doi.org/10.1007/s00064-008-1509-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00064-008-1509-2