Abstract
Background
Health-related quality of life is a multidimensional concept to assess the impact of medical interventions from an individual perspective. This concept is important to evaluate benefits of heart transplantation. This systematic review was conducted to determine (1) posttransplant health-related quality of life in heart transplantation patients and (2) influencing factors of health-related quality of life.
Methods
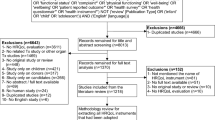
A systematic review of cross-sectional, prospective and mixed methods studies published from November 2007 to November 2017 was conducted on PsycINFO, PSYNDEX and PubMed using a combination of the keywords heart transplantation, heart transplantation patient, quality of life, and health-related quality of life.
Results
A total of 14 studies with a cross-sectional design, 6 studies with a prospective design and 2 mixed-methods studies were identified. The stability of health-related quality of life up to 10 years after transplantation has been reported. Most often generic scales, such as SF-36 (8) and WHOQoL-BREF (7) were used for data collection. Demoralization, depression, pain, gastrointestinal symptoms, sexual dysfunction, and poor oral health influence health-related quality of life negatively, whereas social and family support have a positive impact.
Conclusion
Although health-related quality of life is positively influenced by transplantation, further research regarding gender differences is needed. Disease-specific scales were rarely used.
Zusammenfassung
Hintergrund
Die gesundheitsbezogene Lebensqualität ist ein multidimensionales Konzept, das u. a. der Erhebung des Einflusses von medizinischen Interventionen auf das individuelle Wohlbefinden dient. Herztransplantationen beeinflussen die gesundheitsbezogene Lebensqualität grundlegend. Ziel dieses systematischen Reviews ist, anhand vorliegender Studien einen Überblick über die gesundheitsbezogene Lebensqualität nach Herztransplantationen zu geben und Einflussfaktoren genauer zu beschreiben.
Methoden
Das systematische Review schließt quantitative Studien ein (Querschnittstudien, prospektive Studien und Studien mit gemischtem Design), die zwischen November 2007 und November 2017 veröffentlicht wurden. Das Review wurde auf PsycINFO, PSYNDEX und PubMed mit einer Kombination der Schlüsselwörter „heart transplantation“, „heart transplantation patient“, „quality of life“ und „health-related quality of life“ durchgeführt.
Ergebnisse
Insgesamt 14 Querschnittstudien, 6 prospektive Studien und 2 Studien mit gemischtem Design wurden gefunden. Es zeigt sich eine stabile gesundheitsbezogene Lebensqualität bis zu 10 Jahre nach Herztransplantation. Für die Datenerhebung wurden am häufigsten unspezifische Skalen wie SF-36 und WHOQoL-BREF verwendet. Als negative Einflussfaktoren auf die gesundheitsbezogene Lebensqualität sind Demoralisierung, Depression, Schmerzen, gastrointestinale Beschwerden, sexuelle Dysfunktion und schlechter Zahnstatus zu benennen. Soziale Unterstützung durch die Familie wirkt sich positiv aus.
Diskussion
Defizite in der bisherigen Forschung bestehen vor allem in der fehlenden Betrachtung des Einflusses der Geschlechtszugehörigkeit der Patienten sowie in der seltenen Verwendung krankheitsspezifischer Erhebungsinstrumente.



Similar content being viewed by others
References
Farquhar M (1982) (1995) Elderly people’s definitions of quality of life. Soc Sci Med 41(10):1439–1446
Parmenter TR (1994) Quality of life as a concept and measurable entity. Soc Indic Res 33(1–3):9–46
Raphael D, Renwick R, Brown I, Rootman I (1996) Quality of life indicators and health: current status and emerging conceptions. Soc Indic Res 39(1):65–88
Garratt A, Schmidt L, Mackintosh A, Fitzpatrick R (2002) Quality of life measurement: bibliographic study of patient assessed health outcome measures. BMJ 324(7351):1417
McGee H (2007) Health-Related Quality of Life in Cardiac Patients. In: Cardiovascular prevention and rehabilitation, pp 256–268
Skevington SM, Lotfy M, O’Connell KA (2004) The World Health Organization’s WHOQOL-BREF quality of life assessment: psychometric properties and results of the international field trial. A report from the WHOQOL group. Qual Life Res 13(2):299–310
Hoekstra T, Jaarsma T, Veldhuisen DJ, Hillege HL, Sanderman R, Lesman-Leegte I (2013) Quality of life and survival in patients with heart failure. Eur J Heart Fail 15(1):94–102
Iqbal J, Francis L, Reid J, Murray S, Denvir M (2010) Quality of life in patients with chronic heart failure and their carers: a 3-year follow-up study assessing hospitalization and mortality. Eur J Heart Fail 12(9):1002–1008
Zambroski CH, Moser DK, Bhat G, Ziegler C (2005) Impact of symptom prevalence and symptom burden on quality of life in patients with heart failure. Eur J Cardiovasc Nurs 4(3):198–206
Johansson P, Dahlström U, Broström A (2006) Factors and interventions influencing health-related quality of life in patients with heart failure: a review of the literature. Eur J Cardiovasc Nurs 5(1):5–15
Miller LW (2007) Heart transplantation: indications, outcome, and long-term complications. In: Cardiovascular medicine. Springer, Berlin, Heidelberg, pp 1417–1441
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6(7):e1000097
Von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, Initiative S (2014) The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: guidelines for reporting observational studies. Int J Surg 12(12):1495–1499
Farmer SA, Grady KL, Wang E, McGee EC Jr., Cotts WG, McCarthy PM (2013) Demographic, psychosocial, and behavioral factors associated with survival after heart transplantation. Ann Thorac Surg 95(3):876–883. https://doi.org/10.1016/j.athoracsur.2012.11.041
Shamaskin AM, Rybarczyk BD, Wang E, White-Williams C, McGee E Jr., Cotts W, Grady KL (2012) Older patients (age 65+) report better quality of life, psychological adjustment, and adherence than younger patients 5 years after heart transplant: a multisite study. J Heart Lung Transplant 31(5):478–484. https://doi.org/10.1016/j.healun.2011.11.025
White-Williams C, Grady KL, Myers S, Naftel DC, Wang E, Bourge RC, Rybarczyk B (2013) The relationships among satisfaction with social support, quality of life, and survival 5 to 10 years after heart transplantation. J Cardiovasc Nurs 28(5):407–416. https://doi.org/10.1097/JCN.0b013e3182532672
Tseng PH, Wang SS, Chang CL, Shih FJ (2010) Job resumption status, hindering factors, and interpersonal relationship within post-heart transplant 1 to 4 years as perceived by heart transplant recipients in Taiwan: a between-method triangulation study. Transplant Proc 42(10):4247–4250. https://doi.org/10.1016/j.transproceed.2010.09.063
Saeed I, Rogers C, Murday A (2008) Health-related quality of life after cardiac transplantation: results of a UK National Survey with Norm-based Comparisons. J Heart Lung Transpl 27(6):675–681. https://doi.org/10.1016/j.healun.2008.03.013
Delgado JF, Almenar L, Gonzalez-Vilchez F, Arizon JM, Gomez M, Fuente L, Brossa V, Fernandez J, Diaz B, Pascual D, Lage E, Sanz M, Manito N, Crespo-Leiro MG (2015) Health-related quality of life, social support, and caregiver burden between six and 120 months after heart transplantation: a Spanish multicenter cross-sectional study. Clin Transplant 29(9):771–780. https://doi.org/10.1111/ctr.12578
Galeone A, Kirsch M, Barreda E, Fernandez F, Vaissier E, Pavie A, Leprince P, Varnous S (2014) Clinical outcome and quality of life of patients surviving 20 years or longer after heart transplantation. Transpl Int 27(6):576–582
Kugler C, Tegtbur U, Gottlieb J, Bara C, Malehsa D, Dierich M, Simon A, Haverich A (2010) Health-related quality of life in long-term survivors after heart and lung transplantation: a prospective cohort study. Transplantation 90(4):451–457
Kugler C, Malehsa D, Tegtbur U, Guetzlaff E, Meyer AL, Bara C, Haverich A, Strueber M (2011) Health-related quality of life and exercise tolerance in recipients of heart transplants and left ventricular assist devices: a prospective, comparative study. J Heart Lung Transpl 30(2):204–210. https://doi.org/10.1016/j.healun.2010.08.030
Jakovljevic DG, McDiarmid A, Hallsworth K, Seferovic PM, Ninkovic VM, Parry G, Schueler S, Trenell MI, MacGowan GA (2014) Effect of left ventricular assist device implantation and heart transplantation on habitual physical activity and quality of life. Am J Cardiol 114(1):88–93
Holtzman S, Abbey SE, Stewart DE, Ross HJ (2010) Pain after heart transplantation: prevalence and implications for quality of life. Psychosomatics 51(3):230–236. https://doi.org/10.1176/appi.psy.51.3.230
Aguiar MI, Farias DR, Pinheiro ML, Chaves ES, Rolim IL, Almeida PC (2011) Quality of life of patients that had a heart transplant: application of Whoqol-Bref scale. Arq Bras Cardiol 96(1):60–68
Phan A, Ishak WW, Shen BJ, Fuess J, Philip K, Bresee C, Czer L, Schwarz ER (2010) Persistent sexual dysfunction impairs quality of life after cardiac transplantation. J Sex Med 7(8):2765–2773. https://doi.org/10.1111/j.1743-6109.2010.01854.x
Grandi S, Sirri L, Tossani E, Fava GA (2011) Psychological characterization of demoralization in the setting of heart transplantation. J Clin Psychiatry 72(5):648–654. https://doi.org/10.4088/JCP.09m05191blu
Tung HH, Chen HL, Wei J, Tsay SL (2011) Predictors of quality of life in heart-transplant recipients in Taiwan. Heart Lung 40(4):320–330. https://doi.org/10.1016/j.hrtlng.2009.11.003
Ruzyczka EW, Milaniak I, Przybylowski P, Wierzbicki K, Siwinska J, Hubner FK, Sadowski J (2011) Depression and quality of life in terms of personal resources in heart transplant recipients. Transplant Proc 43(8):3076–3081. https://doi.org/10.1016/j.transproceed.2011.07.012
Kugler C, Bara C, von Waldthausen T, Einhorn I, Haastert B, Fegbeutel C, Haverich A (2014) Association of depression symptoms with quality of life and chronic artery vasculopathy: a cross-sectional study in heart transplant patients. J Psychosom Res 77(2):128–134. https://doi.org/10.1016/j.jpsychores.2014.06.007
Sirri L, Magelli C, Grandi S (2011) Predictors of perceived social support in long-term survivors of cardiac transplant: the role of psychological distress, quality of life, demographic characteristics and clinical course. Psychol Health 26(1):77–94. https://doi.org/10.1080/08870440903377339
Trevizan FB, Miyazaki M, Silva YLW, Roque CMW (2017) Quality of life, depression, anxiety and coping strategies after heart transplantation. Braz J Cardiovasc Surg 32(3):162–170. https://doi.org/10.21470/1678-9741-2017-0029
Milaniak I, Wilczek-Ruzyczka E, Przybylowski P, Wierzbicki K, Siwinska J, Sadowski J (2014) Psychological predictors (personal recourses) of quality of life for heart transplant recipients. Transplant Proc 46(8):2839–2843. https://doi.org/10.1016/j.transproceed.2014.09.026
Jokinen JJ, Hammainen P, Lemstrom KB, Lommi J, Sipponen J, Harjula AL (2010) Association between gastrointestinal symptoms and health-related quality of life after heart transplantation. J Heart Lung Transplant 29(12):1388–1394. https://doi.org/10.1016/j.healun.2010.07.002
Segura-Saint-Gerons R, Segura-Saint-Gerons C, Alcantara-Luque R, Arizon-del Prado JM, Foronda-Garcia-Hidalgo C, Blanco-Hungria A (2012) Perceived influence of oral health upon quality of life in heart transplant patients. Med Oral Patol Oral Cir Bucal 17(3):e409–e414
Riegel B, Moser DK, Carlson B, Deaton C, Armola R, Sethares K, Shively M, Evangelista L, Albert N (2003) Gender differences in quality of life are minimal in patients with heart failure. J Card Fail 9(1):42–48
Strömberg A, Mårtensson J (2003) Gender differences in patients with heart failure. Eur J Cardiovasc Nurs 2(1):7–18
Conway A, Schadewaldt V, Clark R, Ski C, Thompson DR, Doering L (2013) The psychological experiences of adult heart transplant recipients: a systematic review and meta-summary of qualitative findings. Heart Lung 42(6):449–455
Baert A, De Smedt D, De Sutter J, De Bacquer D, Puddu PE, Clays E, Pardaens S (2018) Factors associated with health-related quality of life in stable ambulatory congestive heart failure patients: systematic review. Eur J Prev Cardiol. https://doi.org/10.1177/2047487318755795
Smith H, Taylor R, Mitchell A (2000) A comparison of four quality of life instruments in cardiac patients: SF-36, QLI, QLMI, and SEIQoL. Heart 84(4):390–394
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
E. Tackmann and S. Dettmer declare that they have no competing interests.
This article does not contain any studies with human participants or animals performed by any of the authors.
Caption Electronic Supplementary Material
59_2018_4745_MOESM1_ESM.docx
The supplementary Table 1 provides further information on study design, enrolment criteria, instruments and limitations of the included studies.
Rights and permissions
About this article
Cite this article
Tackmann, E., Dettmer, S. Health-related quality of life in adult heart-transplant recipients—a systematic review. Herz 45, 475–482 (2020). https://doi.org/10.1007/s00059-018-4745-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00059-018-4745-8