Abstract
Background
The prognosis of patients with left ventricular hypertrabeculation/noncompaction (LVHT) and its association with neuromuscular disorders (NMDs) is a controversial topic. The aim of this study was to assess whether the prognosis of LVHT patients is dependent on cardiac phenotype and the presence of NMDs.
Methods
Consecutive patients who were diagnosed with LVHT between 1995 and 2016 were included in the study. Cardiac phenotype was classified according to the recommendations of the European Society of Cardiology as: “dilated” if the left ventricular end-diastolic diameter (LVEDD) was >57 mm and left ventricular fractional shortening (FS) was ≤25%; “hypertrophic” if LVEDD was ≤57 mm, FS > 25%, and left ventricular posterior wall (LVPWT) and interventricular septal thickness (IVST) were both >13 mm; “intermediate” if LVEDD was >57 mm and FS > 25% or if LVEDD was ≤57 mm and FS ≤ 25%; and “normal” if LVEDD was ≤57 mm, FS > 25%, and IVST and LVPWT ≤ 13 mm. Therapy was carried out by the treating physicians.
Results
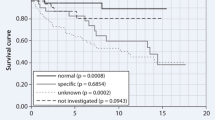
LVHT was diagnosed in 273 patients (80 females, 53 ± 16 years). The phenotype was assessed as dilated in 46%, hypertrophic in 8%, intermediate in 17%, and normal in 29% of the patients. Of these patients, 72% underwent neurological examinations, and an NMD was found in 76%. Over a period of 7.4 years (±5.7), 84 patients died and six underwent cardiac transplantation. The highest mortality rate was observed in the dilated and the lowest in the hypertrophic cardiac phenotype groups. Among the dilated phenotype, mortality was higher in patients with than without NMDs.
Conclusion
Patients with LVHT and dilated cardiac phenotype have a worse prognosis than patients with a hypertrophic or intermediate/normal cardiac phenotype, especially if they suffer from NMDs.
Zusammenfassung
Hintergrund
Die Prognose für Patienten mit linksventrikulärer Hypertrabekulierung/Noncompaction (LVHT) und deren Assoziation mit neuromuskulären Erkrankungen ist ein umstrittenes Thema. Ziel der vorliegenden Studie war es zu untersuchen, ob die Prognose der LVHT-Patienten von dem kardialen Phänotyp und dem Vorliegen neuromuskulärer Erkrankungen abhängig ist.
Methoden
Zwischen 1995 und 2016 wurden alle Patienten mit der Diagnose einer LVHT in die Studie aufgenommen. Der kardiale Phänotyp wurde gemäß den Empfehlungen der European Society of Cardiology als „dilatativ“ klassifiziert, wenn der linksventrikuläre enddiastolische Durchmesser (LVEDD) >57 mm betrug und die linksventrikuläre fraktionelle Verkürzung („fractional shortening“, FS) ≤25 % war; „hypertroph“ bei einem LVEDD ≤57 mm mit FS > 25 % und sowohl linksventrikulärer Hinterwand- (LVPWT) als auch Interventrikularseptumdicke (IVST) >13 mm; „intermediär“ bei LVEDD >57 mm und FS > 25 % oder bei LVEDD ≤57 mm und FS ≤ 25 %; „normal“ bei LVEDD ≤57 mm, FS > 25 % und IVST sowie LVPWT ≤ 13 mm. Die Therapie wurde von den behandelnden Ärzten durchgeführt.
Ergebnisse
Die Diagnose LVHT wurde bei 273 Patienten (80 w., 53 ± 16 Jahre) gestellt. Als dilatiert wurde der Phänotyp bei 46 % klassifiziert, als hypertroph bei 8 %, als intermediär bei 17 % und als normal bei 29 % der Patienten. Eine neurologische Untersuchung wurde bei 72 % der Patienten durchgeführt und eine neuromuskuläre Erkrankung bei 76 % festgestellt. Über einen Zeitraum von 7,4 Jahren (±5,7) verstarben 84 Patienten, und bei 6 erfolgte eine Herztransplantation. Die höchste Mortalitätsrate fand sich in der Gruppe mit dilatativem und die niedrigste in der mit hypertrophem Phänotyp. Bei Patienten mit dilatativem Phänotyp war die Mortalität höher, wenn eine neuromuskuläre Erkrankung vorlag.
Schlussfolgerung
Für Patienten mit LVHT und dilatativem kardialem Phänotyp besteht eine schlechtere Prognose als für Patienten mit hypertrophem oder intermediärem/normalem kardialem Phänotyp, insbesondere bei Vorliegen einer neuromuskulären Erkrankung.


Similar content being viewed by others
Abbreviations
- CED:
-
Cardiac electronic devices
- FS:
-
Fractional shortening
- IVST:
-
Interventricular septal thickness
- LVEDD:
-
Left ventricular end-diastolic diameter
- LVHT:
-
Left ventricular hypertrabeculation/noncompaction
- LVPWT:
-
Left ventricular posterior wall thickness
- NMD:
-
Neuromuscular disorders
- NYHA :
-
New York Heart Association
References
Stöllberger C, Finsterer J, Blazek G (2002) Left ventricular hypertrabeculation/noncompaction and association with additional cardiac abnormalities and neuromuscular disorders. Am J Cardiol 90:899–902
Oechslin E, Jenni R (2011) Left ventricular non-compaction revisited: a distinct phenotype with genetic heterogeneity? Eur Heart J 32:1446–1456
Teo LY, Moran RT, Tang WH (2015) Evolving approaches to genetic evaluation of specific cardiomyopathies. Curr Heart Fail Rep 12:339–349
Aras D, Tufekcioglu O, Ergun K et al (2006) Clinical features of isolated ventricular noncompaction in adults long-term clinical course, echocardiographic properties, and predictors of left ventricular failure. J Card Fail 12:726–733
Lofiego C, Biagini E, Pasquale F et al (2007) Wide spectrum of presentation and variable outcomes of isolated left ventricular non-compaction. Heart 93:65–71
Habib G, Charron P, Eicher JC et al (2011) Isolated left ventricular non-compaction in adults: clinical and echocardiographic features in 105 patients. Results from a French registry. Eur J Heart Fail 13:177–185
Greutmann M, Mah ML, Silversides CK et al (2012) Predictors of adverse outcome in adolescents and adults with isolated left ventricular noncompaction. Am J Cardiol 109:276–281
Stöllberger C, Blazek G, Gessner M et al (2015) Neuromuscular comorbidity, heart failure, and atrial fibrillation as prognostic factors in left ventricular hypertrabeculation/noncompaction. Herz 40:906–911
Stöllberger C, Gerecke B, Engberding R et al (2015) Interobserver agreement of the echocardiographic diagnosis of LV hypertrabeculation/noncompaction. JACC Cardiovasc Imaging 8:1252–1257
Gardin JM, Adams DB, Douglas PS et al (2002) Recommendations for a standardized report for adult transthoracic echocardiography: a report from the American Society of Echocardiography’s Nomenclature and Standards Committee and Task Force for a Standardized Echocardiography Report. J Am Soc Echocardiogr 15:275–290
Elliott P, Andersson B, Arbustini E et al (2008) Classification of the cardiomyopathies: a position statement from the European society of cardiology working group on myocardial and pericardial diseases. Eur Heart J 29:270–276
R Core Team (2013) R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna
Wang C, Takasaki A, Watanabe Ozawa S et al (2017) Long-term prognosis of patients with left ventricular noncompaction—comparison between infantile and juvenile types. Circ J 81(5):694–700
Diwadkar S, Nallamshetty L, Rojas C et al (2017) Echocardiography fails to detect left ventricular noncompaction in a cohort of patients with noncompaction on cardiac magnetic resonance imaging. Clin Cardiol 40:364–369
Ivanov A, Dabiesingh DS, Bhumireddy GP et al (2017) Prevalence and prognosticsignificance of left ventricular noncompaction in patients referred for cardiacmagnetic resonance imaging. Circ Cardiovasc Imaging 10:e6174. https://doi.org/10.1161/CIRCIMAGING.117.006174
Rodrigues JC, Rohan S, Ghosh Dastidar A et al (2017) Hypertensive heart disease versus hypertrophic cardiomyopathy: multi-parametric cardiovascular magnetic resonance discriminators when end-diastolic wall thickness ≥ 15 mm. Eur Radiol 27:1125–1135
Finsterer J, Stöllberger C (2008) Primary myopathies and the heart. Scand Cardiovasc J 42(1):9–24
Cabrera Serrano M, Rabinstein AA (2010) Causes and outcomes of acute neuromuscular respiratory failure. Arch Neurol 67:1089–1094
Kimura K, Takenaka K, Ebihara A et al (2013) Prognostic impact of left ventricular noncompaction in patients with Duchenne/Becker muscular dystrophy—prospective multicenter cohort study. Int J Cardiol 168:1900–1904
Stöllberger C, Blazek G, Bucher E et al (2008) Cardiac resynchronization therapy in left ventricular hypertrabeculation/non-compaction and myopathy. Europace 10:59–62
Qiu Q, Chen YX, Mai JT et al (2015) Effects of cardiac resynchronization therapy on left ventricular remodeling and dyssynchrony in patients with left ventricular noncompaction and heart failure. Int J Cardiovasc Imaging 31:329–337
Penela D, Bijnens B, Doltra A et al (2013) Noncompaction cardiomyopathy is associated with mechanical dyssynchrony: a potential underlying mechanism for favorable response to cardiac resynchronization therapy. J Card Fail 19:80–86
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
C. Stöllberger, C. Wegner, and J. Finsterer declare that they have no competing interests.
This article does not contain any studies with human participants or animals performed by any of the authors.
Rights and permissions
About this article
Cite this article
Stöllberger, C., Wegner, C. & Finsterer, J. Left ventricular hypertrabeculation/noncompaction, cardiac phenotype, and neuromuscular disorders. Herz 44, 659–665 (2019). https://doi.org/10.1007/s00059-018-4695-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00059-018-4695-1