Abstract
Purpose
To assess the impact in pathological complete response (pCR) and outcome of two dose-dense neoadjuvant chemotherapy (DDNC) regimens among different histological subtypes determined by hormonal receptor (HR) and HER2 status in breast cancer patients.
Methods
A total of 127 breast cancer patients were treated with DDNC in two prospective studies. A: adriamycin 40 mg/m2 on day (d) 1 plus paclitaxel 150 mg/m2 and gemcitabine 2,000 mg/m2 on d2 for six cycles (n = 54). B: epirubicin 90 mg/m2, cyclophosphamide 600 mg/m2 on d1 for three cycles, followed by paclitaxel 150 mg/m2 and gemcitabine 2,500 mg/m2 on d1 ± trastuzumab according to HER2 status (n = 73). Histological subtypes of breast cancer were 49 % HR+/HER2−, 17.5 % HR+/HER2+, 13.5 % HR−/HER2+ and 20 % HR−/HER2−.
Results
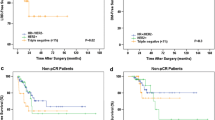
pCR (absence of invasive cells in breast and lymph node) was achieved in 35 patients (28 %). The pCR rate was significantly different between histological subtypes: HR+/HER2− (9 %), HR+/HER2+ (23 %), HR−/HER2+ (50 %), HR−/HER2− (56 %) (p < 0.001). The median follow-up was 81 months (r: 15–150 months). HR−/HER2− tumor subtype had a significantly worse DFS compared to HR+/HER2− (p = 0.02), RH+/HER2+ (p = 0.04) and HR−/HER2+ tumor subtypes (p = 0.02). HR−/HER2− tumor subtype had a significantly shorter OS compared to HR+/HER2− (p = 0.007), RH+/HER2+ (p = 0.05), and HR−/HER2+ (p = 0.03) tumor subtypes. However, no significant difference was observed in DFS and OS among HR−/HER2− tumors that achieved a pCR.
Conclusions
HR−/HER2− and HR−/HER2+ subtypes had a high pCR rate to DDNC. HR−/HER2− tumors had a worse outcome compared to other tumor subtypes but no significant difference was observed among HR−/HER2− tumors that achieved a pCR.
Similar content being viewed by others
References
Perou CM, Sorlie T, Eisen MD, van de Rijn M, Jeffrey SS, Rees CA, et al. Molecular portraits of human breast tumors. Nature. 2000;406:747–52.
Sorlie T, Perou CM, Tibshirani R, Aas T, Geisler S, Johnsen H, et al. Gene expression patterns of breast carcinomas distinguish tumor subclasses with clinical implications. Proc Natl Acad Sci U S A. 2001;98:10869–74.
Sorlie T, Tibshirani R, Parker J, Hastie T, Marron JS, Nobel A, et al. Repeated observation of breast tumor subtypes in independent gene expression data sets. Proc Natl Acad Sci U S A. 2003;100:8418–23.
Rouzier R, Perou CM, Symmans WF, Ibrahim N, Cristofanilli M, Anderson K, et al. Breast cancer molecular subtypes respond differently to preoperative chemotherapy. Clin Cancer Res. 2005;11:5678–85.
Carey LA, Dees EC, Sawyer L, Gatti L, Moore DT, Collichio F, et al. The triple negative paradox: primary tumor chemosensitivity of breast cancer subtypes. Clin Cancer Res. 2007;13:2329–34.
Liedtke C, Mazouni C, Hess KR, André F, Tordai A, Mejia JA, et al. Response to neoadjuvant therapy and long-term survival in patients with triple-negative breast cancer. J Clin Oncol. 2008;26:1275–81.
Untch M, Fasching PA, Konecny GE, Hasmüller S, Lebeau A, Kreienberg R, et al. Pathologic complete response after neoadjuvant chemotherapy plus trastuzumab predicts favorable survival in human epidermal growth factor receptor 2-overexpressing breast cancer: results from the TECHNO trial of the AGO and GBG study groups. J Clin Oncol. 2011;29:3351–7.
Esserman LJ, Berry DA, DeMichele A, Carey L, Davis SE, Buxton M, et al. Pathologic complete response predicts recurrence-free survival more effectively by cancer subset: results from the I-SPY 1 TRIAL–CALGB 150007/150012, ACRIN 6657. J Clin Oncol. 2012;30:3242–9.
Guarneri V, Broglio K, Kau SW, Cristofanilli M, Buzdar AU, Valero V, et al. Prognostic value of pathologic complete response after primary chemotherapy in relation to hormone receptor status and other factors. J Clin Oncol. 2006;24:1037–44.
Colleoni M, Bagnardi V, Rotmensz N, Dellapasqua S, Viale G, Pruneri G, et al. A risk score to predict disease-free survival in patients not achieving a pathological complete remission after preoperative chemotherapy for breast cancer. Ann Oncol. 2009;20:1178–84.
von Minckwitz G, Untch M, Blohmer JU, Costa SD, Eidtmann H, Fasching PA, et al. Definition and impact of pathologic complete response on prognosis after neoadjuvant chemotherapy in various intrinsic breast cancer subtypes. J Clin Oncol. 2012;30:1796–804.
Citron M, Berry D, Cirrincione C, Hudis C, Winer EP, Gradishar WJ, et al. Randomized trial of dose-dense versus conventionally scheduled and sequential versus combination chemo-therapy as postoperative adjuvant treatment for node-positive primary breast cancer: first report of Intergroup Trial C9741/Cancer and Leukemia Group B Trial 9741. J Clin Oncol. 2003;21:1431–9.
Untch M, Möbus V, Kuhn W, Muck BR, Thomssen C, Bauerfeind I, et al. Intensive dose-dense compared with conventionally scheduled preoperative chemotherapy for high-risk primary breast cancer. J Clin Oncol. 2009;27(18):2938–45.
Ellis GK, Barlow WE, Gralow JR, Hortobagyi GN, Russell CA, Royce ME, et al. SWOG 0012, a randomized phase III comparison of standard doxorubicin (A) and cyclophosphamide (C) followed by weekly paclitaxel (T) versus weekly doxorubicin and daily oral cyclophosphamide plus G-CSF (G) followed by weekly paclitaxel as neoadjuvant therapy for inflammatory and locally advanced breast cancer. J Clin Oncol. 2011;29:1014–21.
Therasse P, Mauriac L, Welnicka-Jaskiewicz M, Bruning P, Cufer T, Bonnefoi H, et al. Final results of a randomized phase III trial comparing cyclophosphamide, epirubicin, and fluorouracil with a dose-intensified epirubicin and cyclophosphamide+ filgrastim as neoadjuvant treatment in locally advanced breast cancer: an EORTC-NCIC-SAKK multicenter study. J Clin Oncol. 2003;21:843–50.
Stuart-Harris R, Caldas C, Pinder SE, Pharoah P. Proliferation markers and survival in early breast cancer: a systematic review and meta-analysis of 85 studies in 32,825 patients. Breast. 2008;17:323–34.
de Azambuja E, Cardoso F, de Castro G, Colozza M Jr, Mano MS, Durbecq V, et al. Ki-67 as prognostic marker in early breast cancer: a meta-analysis of published studies involving 12,155 patients. Br J Cancer. 2007;96:1504–13.
Urruticoechea A, Smith IE, Dowsett M. Proliferation marker Ki-67 in early breast cancer. J Clin Oncol. 2005;23:7212–20.
Gianni L, Zambetti M, Clark K, Baker J, Cronin M, Wu J, et al. Gene expression profiles in paraffin-embedded core biopsy tissue predict response to chemotherapy in women with locally advanced breast cancer. J Clin Oncol. 2005;23:7265–77.
Wirapati P, Sotiriou C, Kunkel S, Farmer P, Pradervand S, Haibe-Kains B, et al. Meta-analysis of gene expression profiles in breast cancer: toward a unified understanding of breast cancer subtyping and prognosis signatures. Breast Cancer Res. 2008;10:R65.
Whitfield M, George L, Grant G, Perou CM. Common markers of proliferation. Nat Rev Cancer. 2006;6:99.
Skipper HE. Kinetic behavior versus response to chemotherapy. Natl Cancer Inst monogr. 1971;34:2–14.
Keam B, Im S, Lee K, Han SW, Oh DY, Kim JH, et al. Ki-67 can be used for further classification of triple-negative breast cancer into two subtypes with different response and prognosis. Breast Cancer Res. 2011;13:R22.
Adamo B, Anders C. Stratifying triple-negative breast cancer: which definition(s) to use? Breast Cancer Res. 2011;13:105.
Fasching P, Heusinger K, Haeberle L, Niklos M, Hein A, Bayer CM, et al. Ki67, chemotherapy response, and prognosis in breast cancer patients receiving neoadjuvant treatment. BMC Cancer. 2011;11:486.
Gluz O, Nitz UA, Harbeck N, Ting E, Kates R, Herr A, et al. Triple-negative high risk breast cancer derives particular benefit from dose intensification of adjuvant chemotherapy: results of WSG AM-01 trial West German Group. Ann Oncol. 2008;19:861–70.
Lehmann BD, Bauer JA, Chen X, Sanders ME, Chakravarthy AB, Shyr Y. Identification of human triple-negative breast cancer subtypes and preclinical models for selection of targeted therapies. J Clin Invest. 2012;121:2750–67.
Bauer JA, Chakravarthy AB, Rosenbluth JM, Mi D, Seeley EH. De Matos Granja-Ingram N, et al. Identification of markers of taxane sensitivity using proteomic and genomic analyses of breast tumors from patients receiving neoadjuvant paclitaxel and radiation. Clin Cancer Res. 2010;16(2):681–90.
Juul N, Szallasi Z, Eklund AC, Li Q, Burrell RA, Gerlinger M, et al. Assessment of an RNA interference screen-derived mitotic and ceramide pathway metagene as a predictor of response to neoadjuvant paclitaxel for primary triple-negative breast cancer: a retrospective analysis of five clinical trials. Lancet Oncol. 2010;11:358–65.
Darb-Esfahani S, Loibl S, Müller BM, Roller M, Denkert C, Komor M, et al. Identification of biology-based breast cancer types with distinct predictive and prognostic features: role of steroid hormone and HER2 receptor expression in patients treated with neoadjuvant anthracycline/taxane-based chemotherapy. Breast Cancer Res. 2009;11:R69.
Conflict of interest
No potential conflicts of interest were disclosed.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sánchez-Muñoz, A., Plata-Fernández, Y., Fernández, M. et al. Tumor histological subtyping determined by hormone receptors and HER2 status defines different pathological complete response and outcome to dose-dense neoadjuvant chemotherapy in breast cancer patients. Clin Transl Oncol 16, 548–554 (2014). https://doi.org/10.1007/s12094-013-1116-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12094-013-1116-z