Abstract
Background
Subtrochanteric femur fractures associate with a relatively high complication rate and are traditionally treated operatively with a period of limited weight bearing. Transitioning from extramedullary to intramedullary implants, there are increasing biomechanical and clinical data to support early weight bearing. This multicenter retrospective study examines the effect of postoperative weight bearing as tolerated (WBAT) for subtrochanteric femur fractures. We hypothesize that WBAT will result in a decreased length of stay (LOS) without increasing the incidence of re-operation.
Methods
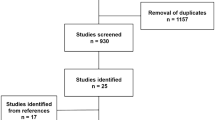
This study assesses total LOS and postoperative LOS after intramedullary fixation for subtrochanteric fractures between postoperative weight bearing protocols across 6 level I trauma centers (n = 441). Analysis techniques consisted of multivariable linear regression and nonparametric comparative tests. Additional subanalyses were performed, targeting mechanism of injury (MOI), Winquist–Hansen fracture comminution, 20-year age strata, and injury severity score (ISS).
Results
Total LOS was shorter in WBAT protocol within the overall sample (7.4 vs 9.7 days; p < 0.01). Rates of re-operation were similar between the two groups (10.6% vs 10.5%; p = 0.99). Stratified analysis identified patients between ages 41–80, WH comminution 2–3, high MOI, and ISS between 6–15 and 21–25 to demonstrate a significant reduction in LOS as a response to WBAT.
Conclusion
An immediate postoperative weight bearing as tolerated protocol in patients with subtrochanteric fractures reduced length of hospital stay with no significant difference in reoperation and complication rates. If no contraindication exists, immediate weight bearing as tolerated should be considered for patients with subtrochanteric femur fractures treated with statically locked intramedullary nails.
Level of evidence
Therapeutic Level III.



Similar content being viewed by others
References
Nieves JW, Bilezikian JP, Lane JM et al (2010) Fragility fractures of the hip and femur: incidence and patient characteristics. Osteoporos Int 21:399–408. https://doi.org/10.1007/s00198-009-0962-6
Ekström W, Németh G, Samnegård E et al (2009) Quality of life after a subtrochanteric fracture. Injury 40:371–376. https://doi.org/10.1016/j.injury.2008.09.010
Waddell JP (1979) Subtrochanteric fractures of the femur: a review of 130 patients. J Trauma 19:582–592
Boyd HB, Lipinski SW (1957) Nonunion of trochanteric and subtrochanteric fractures. Surg Gynecol Obstet 104:463–470
Erez O, Dougherty PJ (2012) Early complications associated with cephalomedullary nail for intertrochanteric hip fractures. J Trauma Acute Care Surg 72:E101–E105
Haidukewych GJ, Berry DJ (2004) Nonunion of fractures of the subtrochanteric region of the femur. Clin Orthop Relat Res 32:185–188
Kinast C, Bolhofner BR, Mast JW, Ganz R (1989) Subtrochanteric fractures of the femur. Results of treatment with the 95 degrees condylar blade-plate. Clin Orthop Relat Res 238:122–130
Anglen JO, Weinstein JN, American Board of Orthopaedic Surgery Research Committee (2008) Nail or plate fixation of intertrochanteric hip fractures: changing pattern of practice. J Bone Jt Surgery-American 90:700–707. https://doi.org/10.2106/JBJS.G.00517
Wiss DA, Brien WW (1992) Subtrochanteric fractures of the femur: results of treatment by interlocking nailing. Clin Orthop Relat Res. https://doi.org/10.1097/00003086-199210000-00032
Beingessner DM, Scolaro JA, Orec RJ et al (2013) Open reduction and intramedullary stabilisation of subtrochanteric femur fractures: a retrospective study of 56 cases. Injury 44:1910–1915. https://doi.org/10.1016/j.injury.2013.08.013
Afsari A, Liporace F, Lindvall E et al (2010) Clamp-assisted reduction of high subtrochanteric fractures of the femur. J Bone Jt Surg Am 92:217–225. https://doi.org/10.2106/JBJS.J.00158
Celebi L, Can M, Muratli HH et al (2006) Indirect reduction and biological internal fixation of comminuted subtrochanteric fractures of the femur. Injury 37:740–750. https://doi.org/10.1016/j.injury.2005.12.022
Riehl JT, Koval KJ, Langford JR et al (2014) Intramedullary nailing of subtrochanteric fractures–does malreduction matter? Bull Hosp Jt Dis 72:159–163
Koval KJ, Friend KD, Aharonoff GB, Zukerman JD (1996) Weight bearing after hip fracture: a prospective series of 596 geriatric hip fracture patients. J Orthop Trauma 10:526–530
Koval KJ, Chen AL, Aharonoff GB et al (2004) Clinical pathway for hip fractures in the elderly: the Hospital for Joint Diseases experience. Clin Orthop Relat Res 425:72–81
Tayrose G, Newman D, Slover J et al (2013) Rapid mobilization decreases length-of-stay in joint replacement patients. Bull Hosp Jt Dis 71:222–226
Wang D, Teddy PJ, Henderson NJ et al (2001) Mobilization of patients after spinal surgery for acute spinal cord injury. Spine (phila.pa.1976) 26:2278–2282
Brumback RJ, Toal TR, Murphy-Zane MS et al (1999) Immediate weight-bearing after treatment of a comminuted fracture of the femoral shaft with a statically locked intramedullary nail. J Bone Joint Surg Am 81:1538–1544
Bailón-Plaza A, van der Meulen MCH (2003) Beneficial effects of moderate, early loading and adverse effects of delayed or excessive loading on bone healing. J Biomech 36:1069–1077
Epstein NE (2014) A review article on the benefits of early mobilization following spinal surgery and other medical/surgical procedures. Surg Neurol Int 5:S66–73. https://doi.org/10.4103/2152-7806.130674
Smeeing DPJ, Houwert RM, Briet JP et al (2015) Weight-Bearing and Mobilization in the Postoperative Care of Ankle Fractures: a systematic review and meta-analysis of randomized controlled trials and cohort studies. PLoS ONE 10:e0118320. https://doi.org/10.1371/journal.pone.0118320
Kubiak EN, Beebe MJ, North K et al (2013) Early Weight Bearing After Lower Extremity Fractures in Adults. J Am Acad Orthop Surg 21:727–738. https://doi.org/10.5435/JAAOS-21-12-727
Cunningham, Brian P.; Zaman, Saif U.; Roberts, Justin; Ortega, Gilbert; Rhorer, Anthony S.; Basmaijian, Hrayr G.; McLemore, Ryan; Parikh, Harsh R.; Miller B (2017) Immediate Weight Bearing as Tolerated Leads to Decreased Length of Stay Compared to Limited Weight Bearing after Intramedullary Fixation for Subtrochanteric Femur Fractures. Orthop Trauma Assoc June:
Marsh JL, Slongo TF, Agel J et al (2007) Fracture and dislocation classification compendium - 2007: orthopaedic trauma association classification, database and outcomes committee. J Orthop Trauma 21:S1–133. https://doi.org/10.1097/00005131-200711101-00001
Winquist RA, Hansen ST (1980) Comminuted fractures of the femoral shaft treated by intramedullary nailing. Orthop Clin North Am 11:633–648
Forward DP, Doro CJ, OToole RV et al (2012) A Biomechanical Comparison of a Locking Plate, a Nail, and a 95° Angled Blade Plate for Fixation of Subtrochanteric Femoral Fractures. J Orthop Trauma 26:334–340. https://doi.org/10.1097/BOT.0b013e3182254ea3
Joglekar SB, Lindvall EM, Martirosian A (2015) Contemporary management of subtrochanteric fractures. Orthop Clin North Am 46:21–35. https://doi.org/10.1016/j.ocl.2014.09.001
Kraemer WJ, Hearn TC, Powell JN, Mahomed N (1996) Fixation of segmental subtrochanteric fractures. A biomechanical study. Clin Orthop Relat Res 332:71–79
Ekström W, Karlsson-Thur C, Larsson S et al (2007) Functional outcome in treatment of unstable trochanteric and subtrochanteric fractures with the proximal femoral nail and the medoff sliding plate. J Orthop Trauma 21:18–25. https://doi.org/10.1097/BOT.0b013e31802b41cf
Robinson CM, Houshian S, Khan LAK (2005) Trochanteric-Entry long cephalomedullary nailing of subtrochanteric fractures caused by low-energy trauma. J Bone Jt Surg 87:2217. https://doi.org/10.2106/JBJS.D.02898
Zhou Z-B, Chen S, Gao Y-S et al (2015) Subtrochanteric femur fracture treated by intramedullary fixation. Chinese J Traumatol 18:336–341. https://doi.org/10.1016/j.cjtee.2015.11.011
French BG, Tornetta P (1998) Use of an interlocked cephalomedullary nail for subtrochanteric fracture stabilization. Clin Orthop Relat Res 348:95–100
Miedel R, Törnkvist H, Ponzer S et al (2011) Musculoskeletal function and quality of life in elderly patients after a subtrochanteric femoral fracture treated with a cephalomedullary nail. J Orthop Trauma 25:208–213. https://doi.org/10.1097/BOT.0b013e3181eaaf52
Egol KA, Dolan R, Koval KJ (2000) Functional outcome of surgery for fractures of the ankle. a prospective, randomised comparison of management in a cast or a functional brace. J Bone Joint Surg Br 82:246–249
Cunningham BP, Dugarte A, McCreary D et al (2017) Immediate weight bearing after operative treatment of bimalleolar and trimalleolar ankle fractures: faster return to work for patients with non-sedentary occupations. Minneapolis, MN
Firoozabadi R, Harnden E, Krieg JC (2015) Immediate weight-bearing after ankle fracture fixation. Adv Orthop 2015:491976. https://doi.org/10.1155/2015/491976
O’Sullivan ME, Bronk JT, Chao EY, Kelly PJ (1994) Experimental study of the effect of weight bearing on fracture healing in the canine tibia. Clin Orthop Relat Res 302:273–283
Simanski CJP, Maegele MG, Lefering R et al (2006) Functional treatment and early weightbearing after an Ankle fracture. J Orthop Trauma 20:108–114. https://doi.org/10.1097/01.bot.0000197701.96954.8c
Heare A, Kramer N, Salib C, Mauffrey C (2017) Early versus late weight-bearing protocols for surgically managed posterior wall acetabular fractures. Orthopedics 40:e652–e657. https://doi.org/10.3928/01477447-20170503-02
Westerman RW, Hull P, Hendry RG, Cooper J (2008) The physiological cost of restricted weight bearing. Injury 39:725–727. https://doi.org/10.1016/j.injury.2007.11.007
Dehghan N, McKee MD, Jenkinson RJ et al (2016) Early weightbearing and range of motion versus non-weightbearing and immobilization after open reduction and internal fixation of unstable ankle fractures. J Orthop Trauma 30:345–352. https://doi.org/10.1097/BOT.0000000000000572
Arazi M, Oğün TC, Oktar MN et al (2001) Early weight-bearing after statically locked reamed intramedullary nailing of comminuted femoral fractures: is it a safe procedure? J Trauma 50:711–716
Jagodzinski M, Krettek C (2007) Effect of mechanical stability on fracture healing—an update. Injury 38:S3–S10. https://doi.org/10.1016/j.injury.2007.02.005
Koval KJ, Sala DA, Kummer FJ, Zuckerman JD (1998) Postoperative weight-bearing after a fracture of the femoral neck or an intertrochanteric fracture. J Bone Joint Surg Am 80:352–356
Hustedt JW, Blizzard DJ, Baumgaertner MR et al (2012) Current advances in training orthopaedic patients to comply with partial weight-bearing instructions. Yale J Biol Med 85:119–125
Funding
No funding was supplied for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Cunningham, B.P., Ali, A., Parikh, H.R. et al. Immediate weight bearing as tolerated (WBAT) correlates with a decreased length of stay post intramedullary fixation for subtrochanteric fractures: a multicenter retrospective cohort study. Eur J Orthop Surg Traumatol 31, 235–243 (2021). https://doi.org/10.1007/s00590-020-02759-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-020-02759-3