Summary
Objective
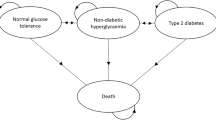
To determine the direct, indirect and intangible costs associated with type 2 diabetes in Italy, 1998. Direct costs were grouped into three main categories, depending on they were due to diabetes, related complications, other unrelated diseases.
Design
An observational, bottom up, prevalence based study (CODE-2: COsts of Diabetes in Europe type 2) was set up to collect information retrospectively with a sample of 1,263 patients.
The sample was stratified, according to main complications types. Resources use, collected via two questionnaires, was measured in monetary terms using a set of costs (when available, like with drugs and GP visits) and tariffs (for the remaining items). Intangible costs were estimated using EQ-5D instrument with the sample patients and then calculating QALYs lost due to the disease.
Setting
Diabetic Centres (DC), that is specialized facilities mainly located in public hospitals, and General Practitioners (GP). GPs were randomly selected, while DCs were selected on a geographic base.
Patients and participants
While enrolling patients (aged at least 30 when diagnosed as type 2 diabetes patients), DCs and GPs were asked to respect the programmed shares for the different complications and the lack of complications. The distribution of the sample patients, with regard both between DCs and GPs and among geographical area was consistent with the distribution of the Italian population.
Main outcome measures and results
The average yearly total cost of a type 2 diabetes patient was 6,072,000 Italian Lire (Lit), while the estimated cost of the whole type 2 diabetes population was about 10,500 billion Lit.
Direct costs accounted for 95.5% of the total. On the whole, they correspond to 6.65% of the total health care expenditure (public plus private) in Italy.
About 60% of the resources value was allocated in hospitals and only 22% ca. was devoted to drugs. Oral anti-diabetics and insulin accounted for less than 20% of the total drug expenditure.
The value of the resources used to treat the illness was 29% of the total direct cost; 39% was the value of the resources for treating the related complications and not less than 32% was required by treatments which could not be related to the illness or its complications.
Estimated intangible costs showed that quality of life in the type 2 diabetes patient is about 10% lower than the average quality level in the general population.
Conclusion
The analysis of the data collected through the CODE-2 study proves that type 2 diabetes has a high social cost, in absolute terms. The major component of such cost is due to the care of the complications, not to the treatment of the illness. In particular, the share of such treatment amenable to drugs is relatively small.
Data reported in the study show that, even from a strictly economic perspective, a policy for the prevention of diabetic complications might be recommendable.
Similar content being viewed by others
Bibliografia
World Bank. World Development Report 1993. Oxford University Press, Oxford, 1993
McCarty D, Zimmet P. Diabetes 1994 to 2010, global estimates and projections. International Diabetes Institute, Melbourne, 1994
Garancini MP. L’epidemiologia del diabete non-insulino-dipendente e della ridotta tolleranza al glucosio. Il diabete in Italia, Editrice Kurtis, 1996
Garancini MP, Lucioni C, Serra G. Il costo sociale del diabete di tipo 2. Una rassegna della letteratura, finalizzata alla realizzazione di uno studio italiano. Il Diabete 11(3): 233–248, 1999
Koopmanschap MA. Cost-of-Illness studies: useful for health policy? Pharmacoeconomics 14(2): 143–148, 1998
Coast J. Developing the QALY Concept. PharmacoEconomics 4(4): 240–246, 1993
Draugalis JLR, Bootman JL, Larson LN, et al. Farmacoeconomia: lo stato dell’arte. Edizione italiana a cura di C. Lucioni, Centro Informazione Sanitaria, 1991
Hodgson TA. Costs of illness in cost-effectiveness analysis: a review of the methodology. Pharmacoeconomics 6(6): 536–552, 1994
Henriksson F, Jönsson B. Diabetes. The cost of illness in Sweden. Stockholm School of Economics, IHE Working Paper, 4, 1997
Brooks R with the EuroQol Group. EuroQol: the current state of play. Health Policy 37: 53–72, 1996
Bradley C. DTQS, Italian Translation. Diabetes Research Group, Department of Psychology, Royal Holloway, University of London, 1997
Nicolucci A, Scorpiglione N, Belfiglio M, et al. Patterns of care of an Italian diabetic population. Diabetic Medicine 14: 158–166, 1997
Garancini MP. L’assistenza al paziente diabetico in Italia negli anni’ 80-’90. Il diabete in Italia, Editrice Kurtis, 1996
ISTAT. Annuario Statistico Italiano. Istituto Nazionale di Statistica, Roma, 1993
Ministero del Tesoro, del Bilancio e della Programmazione Economica. Relazione generale sulla situazione economica del Paese. Istituto Poligrafico e Zecca dello Stato, Roma, 1998
IMS, Servizio Prescrizioni Mediche, 1998
Ministero della Sanità. Prestazioni di assistenza specialistica ambulatoriale erogabili nell’ambito del Servizio Sanitario Nazionale e relative tariffe. Decreto Ministeriale 22 luglio 1996, Supplemento ordinario alla Gazzetta Ufficiale n. 216 del 14 settembre 1996
Bondonio P, Eandi M. I tempi e i costi di lavoro associati al trattamento farmacologico: analisi di alcune opportunità di risparmio. Farmeconomia 2: 36–45, 1995
Regione Lombardia. Ricoveri in Lombardia nel 1997. Direzione Generale Sanità; Sistema Informativo e Controllo Qualità, 1998
ISTAT. Annuario Statistico Italiano. Istituto Nazionale di Statistica, Roma, 1998
Langiano T (a cura di). DRG: strategie, valutazione, monitoraggio. Il Pensiero Scientifico, Roma, 1997
L’Informatore Farmaceutico, luglio 1998 (aggiornamento). OEMF, Milano, 1998
Cooperative Study Group. Diab Nutr Metab 11: 188–193, 1998
Jönsson B, Stålhammer NO. The cost effectiveness of omeprazole and ranitidine in intermittent and maintenance treatment of reflux oesophagitis. The case of Sweden. British Journal of Medical Economics 6: 111–126, 1993
Banca d’Italia. Assemblea Generale Ordinaria dei Partecipanti. Banca d’Italia, Roma, 1999
Koopmanschap MA, Rutten FFH. The impact of indirect costs on outcomes of health care programs. Health Economics 3: 385–393, 1994
Drummond MF, O’Brien BJ, Stoddart GL, Torrance GW. Methods for the economic evaluation of health care programmes. Second Edition. Oxford University Press, 1997
EQ-5D User Guide. EuroQol Business Management, Erasmus University Rotterdam, 1996
OECD. Health Data 98. OECD, Paris, 1998
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
L’Advisory Board Italiano dello Studio CODE-2 è composto da D. Cucinotta, M.P. Garancini, R. Lombardi, R. Giorgino, C. Lucioni, M. Massi-Benedetti, G. Passerini, G. Serra
I peer reviewers, per questo articolo, sono stati coordinati da E. Attanasio
Marchio registrato SmithKline Beecham (CODE-2: Costs of Diabetes in Europe — type 2)
Rights and permissions
About this article
Cite this article
Lucioni, C., Garancini, M.P., Massi-Benedetti, M. et al. Il costo sociale del diabete di tipo 2 in Italia: lo studio CODE-2. Pharmacoeconomics-Ital-Res-Articles 2, 1–21 (2000). https://doi.org/10.1007/BF03320570
Published:
Issue Date:
DOI: https://doi.org/10.1007/BF03320570