Abstract
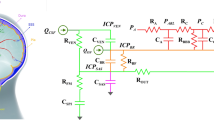
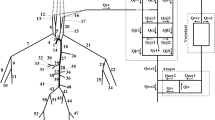
Objective. The purpose of this project was to develop a computer model of cerebrovascular hemodynamics interacting with a pharmacokinetic drug model to examine the effects of various stimuli on cerebral blood flow and intracranial pressure during anesthesia.Methods. The mathematical model of intracranial hemodynamics is a seven-compartment, constant-volume system. A series of resistances relate blood and cerebrospinal fluid fluxes to pressure gradients between compartments. Arterial, venous, and tissue compliance are also included. Autoregulation is modeled by transmural pressure-dependent, arterial-arteriolar resistance. The effect of a drug (thiopental) on cerebrovascular circulation was simulated by a variable arteriolar-capillary resistance. Thiopental concentration was predicted by a three-compartment, pharmacokinetic model. The effect site compartment was included to account for a disequilibrium between drug plasma and biophase concentrations. The model was validated by comparing simulation results with available experimental observations. The simulation program is written in VisSim® dynamic simulation language for an IBM-compatible PC.Results. The model developed was used to calculate the cerebral blood flow and intracranial pressure changes that occur during the induction phase of general anesthesia. Responses to laryngoscopy and intubation were predicted for simulated patients with elevated intracranial pressure and non-autoregulated cerebral circulation. Simulation shows that the induction dose of thiopental reduces intracranial pressure up to 15%. The duration of this effect is limited to less than 3 minutes by rapid redistribution of thiopental and cerebral autoregulation. Subsequent laryngoscopy causes acute intracranial hypertension, exceeding the initial intracranial pressure. Further simulation predicts that this untoward effect can be minimized by an additional dose of thiopental administered immediately prior to intubation.Conclusion. The presented simulation allows comparison of varions drug administration schedules to control intracranial pressure and preserve cerebral blood flow during induction of anesthesia. The model developed can be extended to analyze more complex intraoperative events by adding new submodels.
Similar content being viewed by others
References
Masuzawa T, Fukui Y, Smith NT. Cardiovascular simulation using a multiple modeling method on a digital computer-simulation of interaction between the cardiovascular system and angiotensin II. J Clin Monit 1992; 8: 50–58
Gaba DM, DeAnda A. A comprehensive anesthesia simulation environment: Re-creating the operating room for research and training. Anesthesiology 1988; 69: 387–394
Schwid HA. A flight simulator for general anesthesia training. Comput Biomed Res 1987; 20: 64–75
Philip JH. Gas Man: An example of goal-oriented computer-assisted teaching which results in learning. Int J Clin Monit Comput 1986; 3: 165–173
Fukui Y, Smith NT. Interaction among ventilation, circulation and the uptake and distribution of halothane — Use of a hybrid computer: I. The basic model. Anesthesiology 1981; 54: 107–118
Barnea O, Moore TW, Jaron D. Computer simulation of the mechanically-assisted failing canine circulation. Ann Biomed Eng 1990; 18: 263–283
Braakman R, Sipkema P, Westerhof N. A dynamic nonlinear lumped parameter model for skeletal muscle circulation. Ann Biomed Eng 1989; 17: 593–616
Sharan M, Jones MD Jr, Koehler RC, Traystman RJ, Popel AS. A compartmental model for oxygen transport in brain microcirculation. Ann Biomed Eng 1989; 17: 13–38
Sorek S, Bear J, Karni Z. Resistances and compliances of a compartmental model of the cerebrovascular system. Ann Biomed Eng 1989; 17: 1–12
Pacher RA, Auer LM. Effects of vasospasm in the middle cerebral artery territory on flow velocity and volume flow. A computer simulation. Acta Neurochir 1988; 93: 123–128
Hoffmann O. Biomathematics of intracranial CSF and haemodynamics: Simulation and analysis with aid of mathematical model. Acta Neurochir 1987; 40: 117–130
Zagzoule M, Mark-Vergnes JP. A global mathematical model of cerebral circulation in man. J Biomech 1986; 19: 1015–1022
Hudetz AG, Halsley JH, Horton CR, Conger KA, Reneau DD. Mathematical simulation of cerebral blood flow in focal ischemia. Stroke 1982; 13: 693–700
Marmarou A, Schulman K, Rosende RM. A nonlinear analysis of the cerebrospinal fluid system and intracranial pressure dynamics. J Neurosurg 1978; 48: 332–344
Ursino M. A mathematical study of human intracranial hydrodynamics: Part I. The cerebrospinal fluid pulse pressure. Ann Biomed Eng 1988; 16: 379–401
Ursino M, Giammarco P. A mathematical model of the relationship between cerebral blood volume and intracranial pressure changes: The generation of plateau waves. Ann Biomed Eng 1991; 19: 15–42
Ursino M. Computer analysis of the main parameters extrapolated from the human intracranial basal artery blood flow. Comput Biomed Res 1990; 23: 542–559
Lassen NA. Cerebral blood flow and oxygen consumption in man. Phys Rev 1959; 39: 183–238
Paulson OB, Strandgaard S, Edvinsson L. Cerebral autoregulation. Cerebrovasc Brain Metabol Rev 1990; 2: 161–192
Harper AM, McCulloch J. Cerebral blood flow and cerebrovascular disease. In: Swash M, Kennard C, eds. Scientific basis of clinical neurology. New York: Churchill Livingstone, 1985: 518–532
Aaslid R, Lindegaard KF, Sorteberg W, Nornes H. Cerebral autoregulation dynamics in humans. Stroke 1989; 20: 45–52
Kassell NF, Hitchon P, Gerk M, Sokoll M, Hill T. Alterations in cerebral blood flow, oxygen metabolism, and electrical activity produced by high dose sodium thiopental. Neurosurgery 1980; 7: 598–603
Fragen RJ. Clinical pharmacology and applications of intravenous anesthetic induction agents. In: Bowdle TA, Horita A, Kharasch ED, eds. The Pharmacologic basis of anesthesiology. New York: Churchill Livingstone, 1994: 319–336
Becker KE, Tonnesan AS. Cardiovascular effects of plasma levels of thiopental necessary for anesthesia. Anesthesiology 1978; 49: 197–200
Stanski DR, Maitre PO. Population pharmacokinetics and pharmacodynamics of thiopental: The effect of age revisited. Anesthesiology 1990; 72: 412–422
Hull CJ, English MJM, Sibbald A. Fazadinium and pancuronium: A pharmacodynamic study. Br J Anaesth 1980; 52: 1209–1220
Bekker AY, Von Hagen S, Yarmush J. A Macintosh Hypercard stack to simulate the pharmacokinetics of infusion of intravenous anesthetic drugs (Narsim). Comp Appl Biosci 1991; 7: 531–532
Karayanakis NM. Computer-assisted simulation of dynamic systems with block diagram languages. Boca Raton: CRC Press, 1993: 1–80
Young WL, Ornstein E. Cerebral and spinal cord blood flow. In: Cottrel JE, Smith D, eds. Anesthesia and neurosurgery. Chicago: Mosby Year-Book Inc., 1994: 17–57
Sengupta D, Harper AM, Jennett B. Effect of carotid ligation on cerebral blood flow in baboons; 2. Response to hypoxia and haemorrhagic hypertension. J Neurol Neurosurg Psychiatry 1974; 37: 578–584
Chraemmer-Jorgensen B, Hertel S, Strom J, Hoilund-Carlsen PF, Bjerre-Jepsen K. Catecholamine response to laryngoscopy and intubation. The influence of three different drug combinations commonly used for induction of anaesthesia. Anaesthesia 1992; 47: 750–756
Russel WJ, Morris RE, Frewin DB, Drew SE. Changes in plasma catecholamine concentrations during endotracheal intubation. Br J Anaesth 1981; 53: 837–839
Martin DE, Rosenberg H, Aukburg SJ, Bartkowski RR, Edwards M, Greenhow D, Klineberg P. Low-dose fentanyl blunts circulatory responses to tracheal intubation. Anesth Analg 1982; 61: 680–684
Stoelting RK. Blood pressure and heart rate changes during short-duration laryngoscopy for tracheal intubation: Influence of viscous or intravenous lidocaine. Anesth Analg 1978; 57: 197–199
Tham RQ, Sasse FJ, Ridout VC. Large-scale multiple model for the simulation of anesthesia. In: Moller D, ed. Advanced simulation in biomedicine. New York: Springer Verlag, 1990: pp 173–195
Zwart A, Smith NT, Beneken JEW. Multiple model approach to the uptake and distribution of halothane: The use of analog computer. Computers Biomed Res 1972; 5: 228–238
Ridout VC. Mathematical and computer modeling of physiologic systems. Englewood Cliffs: Prentice Hall 1991: 157–171
Hung OR, Varvel JR, Shafer SL, Stanski DR. Thiopental pharmacodynamics; II. Quantitation of clinical and electroencephalographic depth of anesthesia. Anesthesiology 1992; 77: 237–244
Michenfelder JD. The interdependency of cerebral functional and metabolic effects following massive doses of thiopental in the dog. Anesthesiology 1974; 41: 231–236
Heistad DD, Kontos HA. Cerebral circulation. In: Shepard TY, Aboud FM, eds. Handbook of Physiology: Peripheral Circulation and Organ Blood Flow, vol 3. Bethesda: American Physiological Society, 1983: 137–182
Price HL. A dynamic concepts of the distribution of thiopental in the human body. Anesthesiology 1960; 21: 40–45
Saidman LI, Eger EI. The effect of thiopental metabolism on duration of anesthesia. Anesthesiology 1966; 27: 118–126
Dundee JW, Wyant GM, Clarke RSJ, McKay AC, Bovill JG. Intravenous anaesthesia. New York: Churchill Livingstone, 1988: 69–90
Unadkat JD, Bartha F, Sheiner LB. Simultaneous modeling of pharmacokinetics and pharmacodynamics with nonparametric kinetic and dynamic models. Clin Pharmacol Ther 1986; 40: 86–93
Hull CJ. How far can we go with compartmental models? Anesthesiology 1990; 72: 399–402
Upton RN, Huang YF. Influence of cardiac output, injection time and injection volume on the initial mixing of drugs with venous blood after IV bolus administration to sheep. Br J Anaesth 1993; 70: 333–338
Avram MJ, Sangvi R, Henthorn TK, Krejcie TC, Shanks CA, Fragen RJ, Howard KA, Kaczynski DA. Determinants of thiopental induction dose requirements. Anesth Analg 1993; 70: 10–17
Giffin JP, Cottrell JE, Shwiry B, Harting JH, Epstein J, Lim K. Intracranial pressure, mean arterial pressure, and heart rate following midazolam or thiopental in humans with brain tumors. Anesthesiology 1984; 60: 491–495
Burney RB, Winn R. Increased cerebrospinal fluid pressure during laryngoscopy and intubation for induction of anesthesia. Anesth Analg 1975; 54: 687–690
Van Aken H, Cottrell JE, Anger C, Puchstein C. Treatment of intraoperative emergencies in patients with intracranial disease. Am J Cardiol 1989; 63: 43–58
Fitch W, McDowall DW. Effect of halothane on intracranial pressure gradients in the presence of intracranial spaee occupying lesions. Br J Anaesth 1975; 43: 904–910
Sakabe T, Nakakimura K. Effects of anesthetie agents and other drugs on cerebral blood flow, metabolism, and intracranial pressure. In: Cottrel JE, Smith D, eds. Anesthesia and neurosurgery. Chicago: Mosby Year-Book Inc., 1994: 157–184
Shapiro HM, Wyte SR, Harris AB, Galindo A. Acute intraoperative intracranial hypertension in neurosurgical patients: Mechanical and pharmacologie factors. Anesthesiology 1972; 37: 399–405
Greenbaum RJ, Cooper R, Hulme AS, Mackintosh IK. The effect of induction of anesthesia on intracranial pressure. In: Arias A, ed. Recent progress in anaesthesiology and resuscitation. In: International Congress Series. Amsterdam: Excerpta Medica, 1976: 774–780
Moorthy SS, Greenspan CD, Dierdorf SF, Hillier SC. Increased cerebral and decreased femoral artery blood flow velocities during direct laryngoscopy and tracheal intubation. Anesth Analg 1994; 78: 1144–1148
Shibutani T, Hirota Y, Niwa H, Matsuura H. Cerebral arterial blood flow velocity during induction of general anesthesia: Rapid intravenous induction versus awake intubation. Anesth Prog 1993; 40: 122–126
Miller DR, Martineau RJ, O'Brien H, Hull KA, Oliveras L, Hindmarsh T, Greenway D. Effects of alfentanil on the hemodynamic and catecholamine response to tracheal intubation. Anesth Analg 1993; 76: 1033–1039
Baronia AK, Singh PK, Maheshwari A, Jain VK, Mittal P, Pant KC. Inhaled lidocaine for preventinn of hemodynamic changes in laryngoscopy and intubation. J Neurosurg Anesth 1992; 4: 154–159
White PF, Schlobohm RM, Pitts LH, Lindauer JM. A randomized study of drugs for preventing increases in intracranial pressure during endotracheal suctioning. Anesthesiology 1982; 57: 242–244
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Bekker, A., Wolk, S., Turndorf, H. et al. Computer simulation of cererrovascular circulation: Assessment of intracranial hemodynamics during induction of anesthesia. J Clin Monitor Comput 12, 433–444 (1996). https://doi.org/10.1007/BF02199704
Received:
Revised:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/BF02199704