Summary
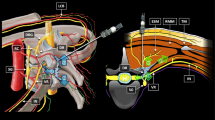
The disorder of neurogenic dysfunction is one of the most important complications of radical hysterectomy. In order to prevent this potential complication, the authors have studied the composition and layers of the pelvic paravisceral structures. The nerve branching and distribution of the pelvic plexus of 12 adult female cadavers were analyzed. From lateral to medial the pelvic paravisceral structure is made up of three layers. The lateral layer is the pelvic visceral fascia, the middle, a vascular layer, and the medial one, a nervous one which consists of the pelvic plexus and subsidiary plexuses. The pelvic plexus and subsidiary plexuses are laid closely to the lateral walls of pelvic organs. The ischial spine was taken as the central point and two perpendicular lines penetrating through the ischial spine were used as the longitudinal axis and transverse axis. According to these land-marks, the pelvic plexus could be divided into three parts: behind the longitudinal axis are the roots of the pelvic plexus, near the longitudinal axis is the uterovaginal plexus, and in front of the longitudinal axis are the branches distributed to bladder and urethra. The pelvic plexus and the uterosacral and cardinal ligaments are closely related. The pelvic and subsidiary plexuses can be damaged in radical hysterectomy and voiding dysfunction may then develop. Some anatomic bases are provided to explain and hopefully prevent this from happening.
Résumé
L'atteinte neurologique de la miction est l'une des complications les plus importantes de l'hystérectomie radicale. Pour éviter les complications induites par l'hystérectomie radicale, les auteurs ont étudié l'anatomie, les branches et la distribution du plexus pelvien sur 12 cadavres féminins adultes. Les structures paraviscérales pelviennes sont formées de 3 couches. La couche externe correspond au fascia pelvien viscéral, la couche moyenne est une couche vasculaire et la couche interne nerveuse est composée du plexus pelvien et de plexi secondaires. Ceux-ci sont situés contre la paroi latérale des organes pelviens. Les repères ont été délimités de la façon suivante ; l'épine sciatique étant le point central, deux lignes croisent ce point comme axe transverse et longitudinal. Ainsi, le plexus pelvien peut être divisé en 3 parties : en arrière de l'axe longitudinal se trouvent les racines du plexus, à coôté de l'axe longitudinal, le plexus utéro-vaginal et en avant de cet axe, les branches de distribution pour l'utètre et la vessie. Il existe des rapports étroits entre le plexus pelvien et les ligaments utéro-sacrés et cardinaux. Le plexus et les plexi secondaires peuvent être endommagés dans les hystérectomies radicales et une dysfonction induite se développer. Quelques bases anatomiques sont étudiées et la façon d'opérer pour protéger le plexus est discutée.
Similar content being viewed by others
References
Forney JP (1980) The effect of radical hysterectomy on bladder physiology. Am J Obstet Gynecol 138: 374–382
Kadar N, Nelson JH (1984) Treatment of urinary incontinence after radical hysterectomy. Obstet Gynecol 64: 400–405
Kadar N, Saliba N, Nelson JH (1983) The frequency, causes and prevention of severe urinary dysfunction after radical hysterectomy. Br J Obstet Gynaecol 90: 858–863
Low JA, Mauger GM, Carmichael JA (1981) The effect of Wertheim hysterectomy upon bladder and urethral function. Am J Obstet Gynecol 139: 826–830
Mundy AR (1982) An anatomical explanation for bladder dysfunction following rectal and uterine surgery. Br J Urol 54: 501–504
Noda K (1985) Preservation of pelvic nerve plexus in radical operation for cervical cancer. Nippon Sanka Fujinka Gakkai Zasshi 37: 313–317
Sasaki H (1980) Studies on neurogenic bladder after radical hysterectomy — significance of preservation of the pelvic nerve plexus. Nippon Gan Chiryo Gakkai Shi 15: 150–160
Seski JC, Diokno AC (1977) Bladder dysfunction after radical hysterectomy. Am J Obstet Gynecol 128: 643–648
Smith PH, Ballantyne B (1968) The neuroanatomical basis for denervation of the urinary bladder following major pelvic surgery. Br J Surg 55: 928–932
Yalla SV, Andride GL (1984) Vesicourethral dysfunction following pelvic visceral ablative surgery. J Urol 132: 503–509
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Tong, XK., Huo, RJ. The anatomical basis and prevention of neurogenic voiding dysfunction following radical hysterectomy. Surg Radiol Anat 13, 145–148 (1991). https://doi.org/10.1007/BF01623891
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/BF01623891