Abstract
Tay-Sachs disease is a rare metabolic disease caused by a deficiency of hexosaminidase A that leads to accumulation of GM2 gangliosides predominantly in neural tissue. Late-onset Tay-Sachs disease variant is associated with a higher level of residual HexA activity. Treatment options are limited, and there are a few described cases who have undergone haematopoietic stem cell transplantation (HSCT) with variable outcome.
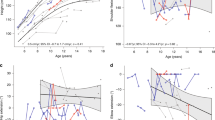
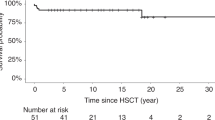
We describe a case of a 23-year-old male patient who presented with a long-standing tremor since 7 years of age. He had gait ataxia, a speech stammer and swallowing problems. His condition had had a static course apart from his tremor that had been gradually deteriorating. Because of the deterioration in his neurological function, the patient had an uneventful, matched-sibling donor bone marrow transplant at the age of 15 years. Eight years post-HSCT, at the age of 23, he retains full donor engraftment, and his white cell beta-HexA of 191 nmol/mg/h is comparable to normal controls (in-assay control = 187). He continues to experience some intentional tremor that is tolerable for daily life and nonprogressive since HSCT.
Conclusion: HSCT is a potential treatment option which might arrest neurodegeneration in patients with LOTS.
Access this chapter
Tax calculation will be finalised at checkout
Purchases are for personal use only
Similar content being viewed by others
Abbreviations
- GA2:
-
GalNAc beta1-4 Gal beta 1-4 Glc-ceramide
- GM2:
-
GalNAc beta 1-4 [NeuAc alpha 2-3] Gal beta 1-4 Glc-ceramide
- Hexa A/B:
-
Hexosaminidase A/B
- HSC:
-
Haematopoietic stem cell
- HSCT:
-
Haematopoietic stem cell transplantation
- Lc3:
-
GlcNAc beta1-3 Gal beta 1-4 Glc-ceramide
- LOTS:
-
Late-onset Tay-Sachs
- LSD:
-
Lysosomal storage disease
- TSD:
-
Tay-Sachs disease
References
Andersson U, Smith D, Jeyakumar M et al (2004) Improved outcome of N-butyldeoxygalactonojirimycin-mediated substrate reduction therapy in a mouse model of Sandhoff disease. Neurobiol Dis 16:506–515
Bley AE, Giannikopoulos OA, Hayden D et al (2011) Natural history of infantile GM2 gangliosidosis. Pediatrics 128(5):1233–1241
Cachon-Gonzalez MB, Wang SZ, Lynch A et al (2006) Effective gene therapy in an authentic model of Tay-Sachs-related diseases. Proc Natl Acad Sci U S A 5:10373–10378
Clarke JT, Mahuran DJ, Sathe S et al (2011) An open-label phase I/II clinical trial of pyrimethamine for the treatment of patients affected with chronic GM2 gangliosidosis (Tay-Sachs or Sandhoff variants). Mol Genet Metab 102:6–12
Codeiro P, Hechtmann P, Kaplan F (2000) The GM2 gangliosidoses databases: allelic variation at the HEXA, HEXB, and GM2A gene loci. Genet Med 2(6):319–327
Godeiro-Junior C, Felicio AC, Benites V et al (2009) Late-onset hexosaminidase A deficiency mimicking primary lateral sclerosis. Arq Neuropsiquiatr 67:105–106
Golebiowski D, van der Bom IMJ, Kwon CS et al (2017) Direct intracranial injection of AAVrh8 encoding monkey beta-N-acetylhexosaminidase causes neurotoxicity in the primate brain. Hum Gene Ther 28(6):510–522
Gravel RA, Clarke JTR, Kaback MM et al (1995) The GM2 gangliosidoses. In: Scriver CR, Beaudet AL, Sly WS et al (eds) The metabolic and molecular basis of inherited disease, 7th edn. McGraw-Hill, New York, pp 2839–2882
Guidotti JE, Akli S, Castelnau-Ptakhine L et al (1998) Retrovirus-mediated enzymatic correction of Tay-Sachs defect in transduced and non-transduced cells. Hum Mol Genet 7:831–838
Jacobs JFM, Willemsen MAAP, Groot-Loonen JJ et al (2005) Allogenic BMT followed by substrate reduction therapy in a child with subacute Tay-Sachs disease. Bone Marrow Transplant 36:925–926
Jeyakumar M, Norflus F, Tifft CJ et al (2001) Enhanced survival in Sandhoff disease mice receiving a combination of substrate deprivation therapy and bone marrow transplantation. Blood 7:327–329
Jeyakumar M, Smith DA, Williams IM et al (2004) NSAIDs increase survival in the Sandhoff disease mouse: synergy with N-butyldeoxynojirimycin. Ann Neurol 56:642–649
Kyrkanides S, Miller JN, Tallents RH et al (2007) Intraperitoneal inoculation of Sandhoff mouse neonates with an HIV-1 based lentiviral vector exacerbates the attendant neuroinflammation and disease phenotype. J Neuroimmunol 188:39–47
Lacorazza HD, Flax JD, Snyder EY, Jendoubi M (1996) Expression of human beta-hexosaminidase alpha-subunit gene (the gene defect of Tay-Sachs disease) in mouse brains upon engraftment of transduced progenitor cells. Nat Med 2(4):424–429
Lee JP, Jeyakumar M, Gonzalez R et al (2007) Stem cells act through multiple mechanisms to benefit mice with neurodegenerative metabolic disease. Nat Med 13:439–447
Mahuran DJ (1995) Beta-hexosaminidase: biosynthesis and processing of the normal enzyme, and identification of mutations causing Jewish Tay–Sachs disease. Clin Biochem 28:101–106
Matsuoka K, Tamura T, Tsuji D et al (2011) Therapeutic potential of intracerebroventricular replacement of modified human β-hexosaminidase B for GM2 gangliosidosis. Mol Ther 19:1017–1024
Myerowitz R (1997) Tay–Sachs disease-causing mutations and neutral polymorphisms in the Hex A gene. Hum Mutat 9:195–208
Neudorfer O, Pastores GM, Zeng BJ et al (2005) Late-onset Tay-Sachs disease: phenotypic characterization and genotypic correlations in 21 affected patients. Genet Med 7:119–123
Neville DC, Coquard V, Priestman DA et al (2004) Analysis of fluorescently labeled glycosphingolipid-derived oligosaccharides following ceramide glycanase digestion and anthranilic acid labeling. Anal Biochem 331:275–282
Norflus F, Tifft CJ, McDonald MP et al (1998) Bone marrow transplantation prolongs life span and ameliorates neurologic manifestations in Sandhoff disease mice. J Clin Invest 101:1881–1888
Osher E, Fattal-Valevski A, Sagie L et al (2015) Effect of cyclic, low dose pyrimethamine treatment in patients with late onset Tay Sachs: an open label, extended pilot study. Orphanet J Rare Dis 10:45
Rosebush PI, MacQueen GM, Clarke JTR, Callahan JW, Strasberg PM, Mazurek MF (1995) Late-onset Tay-Sachs disease presenting as catatonic schizophrenia: diagnostic and treatment issues. J Clin Psychiatry 56(8):347–353
Rountree JS, Butters TD, Wormald MR et al (2009) Design, synthesis, and biological evaluation of enantiomeric beta-N-acetylhexosaminidase inhibitors LABNAc and DABNAc as potential agents against Tay-Sachs and Sandhoff disease. Chem Med Chem 4:378–392
Rowland LP (2010) Progressive muscular atrophy and other lower motor neuron syndromes of adults. Muscle Nerve 41:161–165
Sandhoff K, Christomanou K (1979) Biochemistry and genetics of gangliosidoses. Hum Genet 50:107–143
Sargeant TJ, Wang S, Bradley J, Smith NJ, Raha AA, McNair R, Ziegler RJ, Cheng SH, Cox TM, Cachón-González MB (2011) Adeno-associated virus-mediated expression of β-hexosaminidase prevents neuronal loss in the Sandhoff mouse brain. Hum Mol Genet 20(22):4371–4380
Shapiro BE, Natowicz MR (2009) Late-onset Tay-Sachs disease presenting as a childhood stutter. J Neurol Neurosurg Psychiatry 80:94–95
Shapiro BE, Logigian EL, Kolodny EH, Pastores GM (2008) Late-onset Tay-Sachs disease: the spectrum of peripheral neuropathy in 30 affected patients. Muscle Nerve 38:1012–1015
Shapiro BE, Pastores GM, Gianutsos J, Luzy C, Kolodny EH (2009) Miglustat in late-onset Tay-Sachs disease: a 12-month, randomized, controlled clinical study with 24 months of extended treatment. Genet Med 11:425–433
Shield JP, Stone J, Steward CG (2005) Bone marrow transplantation correcting beta-galactosidase activity does not influence neurological outcome in juvenile GM1-gangliosidosis. J Inherit Metab Dis 28(5):797–798
Suzuki K (1991) Neuropathology of late-onset gangliosidoses. Dev Neurosci 13:205–210
Tropak MB, Reid SP, Guiral M, Withers SG, Mahuran D (2004) Pharmacological enhancement of beta-hexosaminidase activity in fibroblasts from adult Tay-Sachs and Sandhoff patients. J Biol Chem 279:13478–13487
Wada R, Tifft CJ, Proia RL (2000) Microglial activation precedes acute neurodegeneration in Sandhoff disease and is suppressed by bone marrow transplantation. PNAS 97:10954–10959
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Additional information
Communicated by: Gregory M. Pastores, MD
Appendices
Synopsis
HSCT is a potential disease modifying therapy for late-onset Tay-Sachs disease.
General Rules
Details of the Contributions of Individual Authors
KMS conception and design, analysis and interpretation of data, drafting the chapter and revising the chapter critically for important intellectual content.
SHM conception and design, analysis and interpretation of data, drafting the chapter and revising the chapter critically for important intellectual content.
JEW conception and design and analysis and interpretation of data.
CJH revising the chapter critically for important intellectual content.
HC acquisition of data and interpretation of data.
DP conception and design, analysis and interpretation of data, drafting the chapter and revising the chapter critically for important intellectual content.
FP revising the chapter critically for important intellectual content.
SJ acquisition of data and revising the chapter critically for important intellectual content.
AJ acquisition of data and revising the chapter critically for important intellectual content.
RW conception and design, analysis and interpretation of data, drafting the chapter and revising the chapter critically for important intellectual content.
All authors read and approved the manuscript before submission.
The Name of the Corresponding Author
Karolina M. Stepien.
The Mark Holland Metabolic Unit.
Adult Inherited Metabolic Disorders.
Salford, M6 8HD.
Tel 0161 2064365.
A Competing Interest Statement
KS received travel grants from Genzyme, Shire, BioMarin, Amicus and Alexion. She has conflict of interest for this publication.
SHL has no conflict of interest for this publication.
JEW has no conflict of interest for this publication.
CJH is a consultant for Actelion, BioMarin, Chiesi Inventiva, Sanofi, Genzyme and Shire and is owner director of FYMCA Medical Ltd.
HC has no conflict of interest for this publication.
DP has no conflict of interest for this publication.
FP is a co-founder of IntraBio and consultant to IntraBio, Actelion and Orphazyme. She has conflict of interest for this publication.
SJ has no conflict of interest for this publication.
AJ has no conflict of interest for this publication.
RW has no conflict of interest for this publication.
Details of funding: N/A.
Details of ethics approval: patient’s consent to bone marrow transplant includes consent to use of transplant outcome data.
A patient consent statement: patient’s consent was obtained.
Documentation of approval from the Institutional Committee for Care and Use of Laboratory Animals (or comparable committee): N/A.
Guarantor: RW.
Rights and permissions
Copyright information
© 2017 Society for the Study of Inborn Errors of Metabolism (SSIEM)
About this chapter
Cite this chapter
Stepien, K.M. et al. (2017). Haematopoietic Stem Cell Transplantation Arrests the Progression of Neurodegenerative Disease in Late-Onset Tay-Sachs Disease. In: Morava, E., Baumgartner, M., Patterson, M., Rahman, S., Zschocke, J., Peters, V. (eds) JIMD Reports, Volume 41. JIMD Reports, vol 41. Springer, Berlin, Heidelberg. https://doi.org/10.1007/8904_2017_76
Download citation
DOI: https://doi.org/10.1007/8904_2017_76
Received:
Revised:
Accepted:
Published:
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-662-58080-6
Online ISBN: 978-3-662-58081-3
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)