An integrated mHealth model for type 2 diabetes patients using mobile tablet devices
Sora Park, PhD1, Sally Burford, PhD1, Leif Hanlen, PhD2, Paresh Dawda, MBBS/DRCOG3, Paul Dugdale, PhD/FAFPHM4, Christopher Nolan, MBBS/PhD5, John Burns, Adjunct Professor6
1News & Media Research Centre, University of Canberra, ACT, Australia; 2Data61, University of Canberra, Australian National University, ACT, Australia; 3Ochre Health Medical Centre, ACT, Australia; 4College of Medicine, Biology & Environment, Australian National University, ACT, Australia; 5College of Medicine, Biology & Environment, Australian National University, Canberra Hospital, ACT, Australia; 6University of Canberra, ACT, Australia
Corresponding Author: sora.park@canberra.edu.au
Journal MTM 5:2:24–32, 2016
doi: 10.7309/jmtm.5.2.4
Background: Ease of use, proximity to the user and various health maintenance applications enable mobile tablet devices to improve patient self-management. With mobile phones becoming prevalent, various mobile health (mHealth) programs have been devised, to improve patient care and strengthen healthcare systems.
Aims: This study explored how mHealth programs can be developed for type 2 diabetes patients through a co-design participatory workshop between practitioners and researchers. The aim was to design a mHealth pilot program from the input.
Methods: A co-design workshop was conducted with 15 participants, including general practitioners, specialists, nurses and a multidisciplinary research team. Participants generated 31 statements in response to a trigger question and engaged in a structured discussion. Thematic cluster analysis was conducted on the statements and discussions.
Results: Through the analysis, patients’ self-management and health system integration emerged as the main topics. Further analysis revealed that there were two distinct areas of patient self-management; ‘compelled’ and ‘empowered’.
Conclusion: With the results, a loose-knit mHealth pilot program was developed wherein patients with various levels of conditions and digital skills could be incorporated. In order to encourage sustainable changes, practitioners proposed that mobile devices must be situated in the patients’ everyday settings and that digital training should be provided.
Introduction
According to the World Health Organization, the number of diabetes patients worldwide will have reached 366 million by 2030.1 In Australia, diabetes is the sixth leading cause of death and the death rate continues to rise.2 The diagnosis and treatment of diabetes are crucial, as the condition may pose other risks such as heart disease, stroke, blindness, and kidney failure. Type 2 diabetes results from the body’s ineffective use of insulin and accounts for approximately 90% of all diabetes diagnoses. Simple lifestyle changes such as maintaining an optimal body weight, engaging in physical activity and adopting a healthy diet are essential to the management of type 2 diabetes.1
Diabetes is a chronic condition that needs special attention to diet and exercise that involves patients’ active self-management.3 Self-management of an illness requires a considerable level of knowledge, discipline and self-regulation. For this reason, prescribed activities are not solely determined by medical factors. For example, the health outcomes of blood glucose self-testing among type 2 diabetes patients have not been clearly established. Nevertheless, the practice is beneficial because it can contribute to the patients’ self-management strategies by giving patients the opportunity to reflect on their condition.4 Characteristics of successful patients include accountability, motivation for change and active participation. Peer support and community resources are also effective methods of engaging patients. A longitudinal study on relationship between the patients’ social networks and their self-management of chronic illness shows that social involvement with wider resources supports not only the day-to-day tasks but also helps manage long term conditions and the patients’ emotional well-being.5
With mobile phones becoming prevalent, various mobile health (mHealth) programs have been devised to improve patient care and strengthen healthcare systems. Ease of use, portability and ubiquity all point to the potential of mobile devices for use in preventing, diagnosing and treating illnesses, as well as increasing access to health services and lowering costs. The benefits of using mobile devices are in the continuous access they provide and their proximity to users. Mobile devices are both ‘always on’6 and ‘always with’ the user.7 This enables seamless healthcare service delivery, while requiring active participation and control by the users.
There are many potential benefits of mHealth programs. Mobile applications (apps) may be used for positive health promotion, physical fitness, treatment adherence and disease management. Mobile technologies can also be used for diagnosis, complying with treatment, obtaining patient information and increasing administrative efficiency.8 As part of the DC Chronic Care Initiative, Katz, Mesfin and Barr conducted a mobile phone-assisted diabetes self-management project.9 Thirty-two type 2 diabetes patients were given mobile phones with subscription and were connected to an interactive platform for patients and health care providers to track blood glucose and receive real-time feedback and diabetes information. Although half of the patients dropped out in the middle of the study, among those who remained hospital emergency room visits and hospitalization were reduced. Technology can support patients’ self-management, for example, by enabling self-monitoring of blood glucose levels. However, it is difficult to sustain the behaviour.10
An important element of diabetes care is the patients’ active involvement in their self-management.11–13 The ability varies from person to person and evolves over time.14 The contextual nature of health behavior influences an individual’s level of engagement.15
The digital environment that affects the user’s engagement and the sustainability of the patient’s behavioural change must be taken into consideration. However, it has not been established whether behavioural change techniques provided by digital devices are effective in the long run.16 A meta-analysis of 85 internet intervention programs concludes that they were mostly effective especially if they were based on the theory of planned behaviour. Including more techniques and using additional communication methods were found to enhance the effects.17 Effective health interventions need to be based on theories of behavioural change that incorporate specific techniques. Intervention programs usually entail a controlled experiment where subjects are randomly assigned to a trial. The changes in behaviour are measured after the trial and the effectiveness of the program is evaluated. While such models provide efficient ways to implement medical treatments, the limits of such experiments are that they cannot explain the broader link to other socio-cultural factors that come into play when patients are dealing with their health conditions. A more holistic examination of the multitude of factors that influence patients’ engagement with digital technologies is necessary.
Most mHealth studies examine the effectiveness of interventions delivered via mobile devices, using controlled trials where variables can be observed in isolation.18 Such models offer limited means for the observation of patients’ long-term behavioural changes. Digital devices are used within the user’s socio-cultural context and mHealth programs cannot be separated from other uses of the devices. However, little is known about the process of how patients adapt to the devices used in mHealth programs. In order to implement a sustainable program, we need to carefully examine how mHealth tools are adopted and utilized by users within the broader social context.
It is crucial to know the affordances as well as how users engage with digital technologies.
Easy and instantaneous access to information is one of the strengths of mobile devices. The internet is known to be effective in providing dietary information, accessing electronic medical records, education and visualising data. Mobile phones are good for uploading glucose levels, receiving text messages from clinicians and running self-management applications.19
Mobile tablet devices are not as widely used as smartphones or computers. They are positioned in-between computers and phones in that they afford large enough screens for users to engage in lengthy information seeking but are also highly portable.7 The portability within a designated area such as the home or office, differentiate them from computers.20 The proximity to the user, continuous Internet access and ease of use can be used advantageously when devising self-management programs.
Research questions
This study adopted an exploratory approach because little research has been conducted specifically on mobile tablet devices in mHealth. Mobile tablet devices can be positioned between mobile phones and computers and offer a unique experience to users.20 However, like any other technologies, the adoption is complex because it does not occur in a vacuum, and it involves interaction with the user over time.21 Technologies are constantly advancing; therefore, implementation of new programs should be flexible and contextual.22 How users – practitioners and patients – perceive of and interact with the technologies is crucial to implementing a successful digital health program. As a first step towards developing a sustainable mHealth program, the aim of this paper was to identify ways in which these devices can be situated within mHealth from the practitioners’ viewpoint. This will set the initial frame for further investigation into how mHealth programs can be embedded into the overall management of chronic illness, in this case, type 2 diabetes.
The following research questions were established:
RQ1. According to practitioners what are the potential uses of mobile tablet devices in managing type 2 diabetes?
RQ2. What areas do practitioners perceive of to be particularly beneficial to patients in their uses of mobile tablet devices to manage type 2 diabetes?
Methods
In order to facilitate an environment where the new technologies are embraced by users and benefit them, a co-design method was adopted as a first step in developing a mHealth pilot program for diabetes patients. Using a qualitative approach, this study commenced with a broadly defined concept of mHealth in order to explore the elements of a successful technology adoption in self-management and health care.
A practitioner co-design workshop (N =15) involving GPs, nurses, and the research team was held at a local GP Super Clinic# on July 22, 2014. The aim of the workshop was to develop a framework of a year-long mHealth pilot program. This paper reports on the practitioners’ perspectives on how mHealth may be enabled in primary care settings. We initially invited all of the GPs and nurses at the Clinic (N=16) of which 11 attended.
The workshop was carefully structured so that all participants could fully contribute regardless of their role in the discussion. Too much or too little information may lead to premature decision-making and poorly conceptualised designs.23 Structured dialogue methods are suitable for use in complex situations where the group cannot meet regularly to discuss the project and have not collaborated before, but share a common goal. A workshop facilitating a structured dialogue was optimal for the purposes of this study, because of the complexity of the prevailing issue and also due to the diverse expertise of participants.
Prior to the workshop, a trigger question was posed in order to ensure efficient management of the discourse; the participants were required to respond with up to two statements. The trigger question, “how could you and your diabetes type 2 patients use a mobile tablet to manage this health condition?” was sent out to the practitioner participants and they were asked to bring their draft statements to the workshop. During the fairly open discussion, the facilitator deliberately asked all participants to present and explain their responses. This method enabled participants not only to engage in the discourse equally but also to appreciate the diversity in the responses given.
A total of 31 statements were collected and categorized by themes. Eleven practitioners participated in the discussion, including seven GPs, one specialist, and three nurses. Throughout this paper, pseudonyms are used for anonymity. Six research team members participated in the dialogue to ensure diversity in the viewpoints presented and to maintain focus on the research goal. Two practitioners were also research team members, but are indicated as practitioners in this paper. In the analysis, the non-practitioner research team members are identified as R1-R4. These researchers are scholars with expertise in communication, health, information studies and technology.
During the first round of discussion, participants were given the opportunity to clarify and elaborate on their statements that they supplied before open discussion. The written statements that the participants and the discussions that followed during the workshop were both taken into account when identifying the themes. The written statements were collected and compiled together. Participants had the opportunity to clarify or modify their statements during the discussion. The research team took notes during the discussion and added the text to the list of statements. The statements and notes were qualitatively analysed by two research team members initially. Statements were grouped into themes during several iterations. The recurring themes were then categorized into items that reflect different aspects of a mHealth program. The themes and subcategories were shared with the team members for validation. The research was approved by the Human Ethics Committee at the lead researcher’s organization.
Results
Fifteen participants generated 31 statements (see Appendix for the list) in response to the trigger question. Using qualitative thematic clustering, two broad topics were identified: patient engagement and health system integration (Table 1). Practitioners viewed mobile tablet devices to be mainly used by the patient in their self-management but also envisioned a scope for mobile technologies to provide seamless access to the existing digital health systems.

Table 1: mHealth benefits
The patient self-management topic comprised the majority of the statements, with 24 of 31 statements related to the devices’ use for patient self-management. Self-management, then, was divided into two sub-topics depending on patients’ level of engagement, which was named as ‘compelled’ and ‘empowered’. Participants differentiated activities that are required by the doctors such as recording blood glucose levels, which patients often find burdensome. We labelled such routine activities as ‘compelled’. Other activities which patients are more engaged with we labelled as ‘empowered’. The general consensus was that active information seeking, communication, self-reflection, and education can empower patients to engage in sustainable self-management activities. On the other hand, healthcare system integration implies a broader policy that facilitates a shift to a digitalised healthcare delivery. Statements for each category are summarised in Table 1.
Patients’ use of mobile tablet devices for self-management can be understood within a broad context of their overall digital engagement. Identification of diversified uses of mobile tablet devices is an important step towards the design of effective mHealth programs. Mobile devices are intended to serve many purposes, including self-management. Two sub-topics related to self-management activities emerged from the discussions, namely, assistance with day-to-day activities required for routine diabetes management, and patient empowerment aimed at enhancing autonomous self-management. The two sub-topics – ‘compelled’ and ‘empowered’ – were identified as related, yet conceptually distinct.
Mobile devices as tools for compelled self-management
Mobile devices can be effectively used by patients to facilitate the management program prescribed for diabetes patients, such as keeping record of blood glucose levels (BGL) and other biometric data. It can also be used as a tool to provide easy access to authoritative information. When first diagnosed, patients receive basic information from health practitioners, such as what to do, avoid, and not eat. In a mHealth program, basic knowledge and record keeping should be readily accessible to patients via the devices (R1).
However, simple recording and obtaining knowledge do not automatically constitute effective self-management. Patients must constantly track, look back on, and adjust their behaviour. Mobile devices have the potential to bridge the gap between knowledge and behavioural change by improved tracking and recording, compared to the pen-and-paper method. Use of mobile apps as constant reminders and feedback on dietary information about the food intake is an immediate benefit. The devices can also be used to “coordinate reminders for multiple appointments” (R2).
Among the compelled activities, checking and recording blood glucose levels and getting access to authoritative information online were suggested as activities that could be conducted on a mobile tablet device.
Mobile devices as patient empowerment tools
Nevertheless, several challenges must be addressed prior to the implementation of mHealth programs. While it is important “to respond to prompts [for] correct treatment times” (Alyssa) and use the “built-in reminders such as when to take pills or exercise” (Cooper), “there has to be something in it for them (as far as outcomes are concerned); they have to be doing it for themselves” (Declan). Beyond the immediate benefits, patients must want to continue to use the device after the novelty phase (Mason). For the device to be empowering, practitioners suggested a need for various activities that are more than simple day-to-day self-management. For example, patients may engage more meaningfully with their self-management when participating in educational activities, keeping reflective journals, and managing customised exercise or diet routines. Empowerment can also occur when patients share information or receive social support. By using the device, patients may have “time to realize what effect their food and diet can have” (Declan). The mHealth program can enable patients to exercise “autonomy with their health and be more proactive, which will help us (staff) tend better to the patients” (Kira). The devices can also be used to coordinate activities or support planning (Peter).
The device can be utilized as an “educational package” (Colin) providing general information on type 2 diabetes, what it is, and why it must be controlled and managed. It can serve as a preventive measure to screen further complications. Accessing information through online resources could also facilitate autonomous management. Patients often need to “get information on what to do in any situation” (Kaitlin) or “communicate with others to share information and experience” (R3). On-screen availability of the information was considered a “better format to help them understand their condition” (Daniel).
Managing diabetes can be challenging because it requires a certain level of self-discipline and consistency. Patients have to constantly monitor their activities or record their BGL just to maintain their daily lives. They have to learn to live with their health conditions. The practitioners acknowledged the importance of patients’ autonomy. Patients can address the daily challenges by learning more about the relevant health condition, sharing information, reflecting on the difficulties, and learning new coping mechanisms. In general, acquisition of new knowledge and learning new ways to manage a condition are successful pathways to self-care. When designing or evaluating an mHealth diabetes management program, it is crucial to incorporate patients’ sense of autonomy and independence (Colin) and instil a sense of “owning their disease” (Kira), by allowing them to “turn into their own researcher, with the device constantly giving them feedback” (R4).
Patients’ varying digital skills and attitudes towards the technology also need to be taken into account. Possible attrition during the pilot program must also be considered (Kaitlin).
The ultimate question is whether mHealth self-management programs can change patients’ behaviour. Many patients experience fatigue in their self-care and often “cannot maintain or control their lifestyles” (Emma). One of the aims of this project is to “identify the types of people whom mHealth would appeal to” (Peter).
Four additional empowerment activities—diet and nutrition, exercise, keeping a journal, and communicating— were suggested as activities that are essential to sustainable self-management that could be conducted with mobile tablet devices.
Incorporating mobile tablet devices seamlessly into the current healthcare delivery system
By connecting patients via mobile devices to online health systems, practitioners can keep track of patients records closely (Audrey). The devices can fill the void between doctors’ visits and provide patients with “a sense of access and care in-between consultations” (R2).
The addition of the device to patients’ various health management options could, over time, enhance the overall digital environment, if both doctors and patients are tolerant of digital health systems. “There is a national e-record system, but only about one third of patients have signed up and nobody really uses it. For this to be effective, practitioners have to use it first” (Declan). Seamless introduction of digital technologies via easy accessible mobile devices into the healthcare delivery system could encourage the online system. Furthermore, if mobile devices are used prevalently among patients and they increasingly demand access to e-records, this could be a trigger for a wider adoption (R2). Potentially, mobile devices may serve as a gateway to other digital health systems (R3).
Discussion
As outlined in Table 1, a mHealth model of patient self-management was suggested. And for mHealth programs to be effective, patients must perceive the technologies to be beneficial to their daily diabetes management as well as have the capability to utilise the tools on these devices. Patients need to be comfortable in using the digital tools available to them. The practitioners proposed an open and loose-knit pilot program where patients can learn, explore, and make use of the devices in long term. Positioning the devices within the context of the patients’ every day context was viewed as a precondition for effective engagement with the devices, and eventually successful mHealth program outcomes.
Among the uses of the devices, practitioners’ suggestions were grouped into six activities. Of these, measurement of biometric information (e.g., BGL) through mobile apps and getting access to credible websites are named as “compelled” activities. These activities are necessitated by the patients’ diabetes condition and often required by their GPs. Four additional activities—diet and nutrition, exercise, keeping a journal, and communicating—are labelled as “empowered” activities. These are activities that are essential to maintaining the patients’ health but need further engagement from the patient in order to be effective. The concept, “patient empowerment,” that emerged from the discussions is an important element of sustaining self-management which can be a challenge to diabetes patients.
When implementing a mHealth program the following needs to be considered. First, due to the complexity of adopting digital technologies, instead of applying a clinical intervention model in short term, a looser model of self-management that is embedded into the patients’ everyday lives should be designed. To date, theoretical causal inferences about emerging technologies are often limited. Second, technology adoption does not occur in a vacuum; it is usually intertwined with other aspects of life and users’ needs. A broader approach is needed to understand how people engage with new technologies. When technology adoption is required in the program, the user’s context needs to be considered. Third, when appropriated by users, technologies result in divergent outcomes. What is meaningful and effective for one user is not necessarily so for another. Thus, a diversified approach, rather than a one-size-fits-all strategy, is necessary during implementation of mHealth programs. This is particularly the case if the patients’ levels of digital literacy are varied.
At the co-design workshop, practitioner participants agreed that the pilot program should allow patients sufficient autonomy and encourage them to try new tools independently. Rather than implementing a highly structured intervention program, discussions at the workshop suggest that an initial exploratory program, where patients are invited to engage in various digital activities relating to their health management, that includes sufficient digital literacy training and technical support, would be more likely to induce behavioural changes among diabetes patients in the long term.
A limitation of this paper is that only the practitioners were involved in the design of the program. A fuller picture of how patients engage with mobile devices for their self-management can be painted after observing the patient participants for a year in the next step of the project. Nevertheless, this paper contributes to the body of literature in mHealth where new technologies are constantly introduced into health care. It emphasises the importance of interaction between technology and user (patient) during the implementation of an mHealth program. The integration of digital technologies, appropriate programs of lifestyle changes, and active engagement of patients into the model was suggested as crucial elements of a sustainable mHealth program. New technological systems must be accompanied by a shift that occurs at all levels, including technical and organizational systems, patient participation, and practitioner support.
The next step of the research is to conduct a pilot program with type 2 diabetes patients where participants are to be given iPads preinstalled with mobile apps to help manage their health condition. Mobile tablet devices have larger screens which may be favourably accepted by novice users of digital technologies. Compared to iPads, mobile phones are more portable but the uses may be limiting due to the small screen size.20
Conclusion
This paper reports findings from a co-design workshop involving healthcare practitioners and a multidisciplinary research team. The first research question asked what practitioners perceived to be potential uses of mobile tablet devices in managing type 2 diabetes. Broadly, integration into the existing healthcare delivery system was identified as an important function of mobile tablet devices. More importantly, most practitioners suggested that mobile tablet devices will benefit the patient if used as the patients’ motivational and self-management tools. The second research question was related to how patients could use the device to self-manage their condition. In this, practitioners suggested measurement and recording activities as an alternative to paper-based method. Empowering the patient by transferring a sense of ownership and autonomy was also regarded as an important role of mHealth.
From this result, we proposed a co-design model where an open mHealth program can be explored. In the proposed mHealth program, patients with various levels of digital skills are to be given adequate time to adapt to the devices and applications, ultimately giving them an opportunity to learn and appropriate the technology independently. Since patients come with different levels of digital literacy, the approach should be individualized where each user can learn at their own pace. During the implementation of the mHealth pilot program, adequate training and support must be provided in addition to the access to devices and digital tools. Such efforts to enable digital engagement should be seamlessly integrated into the mHealth program of self-management, whereby patients can comfortably engage in both ‘compelled’ and ‘empowered’ activities in order to find effective ways of managing their diabetes condition.
References
1. Diabetes Fact Sheet. Geneva: World Health Organization, 2014. http://www.who.int/mediacentre/factsheets/fs312/en/
2. Causes of Death, Australia, 2011 Canberra: Australian Bureau of Statistics, 2013. http://www.abs.gov.au/ausstats/abs@.nsf/Lookup/3303.0Chapter42011
3. Coyle ME, Francis K, Chapman Y. Self-management activities in diabetes care: a systematic review. Australian Health Review. 2013;37(4):513–22. ![]()
4. Bond CS, Hewitt-Taylor J. How people with diabetes integrate self-monitoring of blood glucose into their self-management strategies. Informatics in Primary Care. 2014;21(2):64–9. ![]()
5. Reeves D, Blickem C, Vassilev I, Brooks HAK, et al. The Contribution of Social Networks to the Health and Self-Management of Patients with Long-Term Conditions: A Longitudinal Study. PLoS ONE. 2014;9(6):e98340. ![]()
6. Turkle S. Always-on/always-on-you: The tethered self. In: Katz J, editor. Handbook of mobile communication studies Cambridge: MIT Press; 2008. p. 121–38.
7. Park S. Always on and always with mobile tablet devices: A qualitative study on how young adults negotiate with continuous connected presence. Bulletin of Science. Technology & Society. 2013;33(5-6):182–90. ![]()
8. Fiordelli M, Diviani N, Schulz PJ. Mapping mHealth Research: A Decade of Evolution. Journal of Internet Medical Research. 2013;15(5). ![]()
9. Katz R, Mesfin T, Barr K. Lessons From a Community-Based mHealth Diabetes Self-Management Program: “It’s Not Just About the Cell Phone”. Journal of Health Communication. 2012;17(sup1):67–72. ![]()
10. Chen L, Chuang LM, Chang CH, Wang CS, Wang IC, Chung Y, … Lai F. Evaluating self-management behaviors of diabetic patients in a telehealthcare program: Longitudinal study over 18 months. Journal of Medical Internet Research, 2013:15(12). ![]()
11. Coyle ME, Francis K, Chapman Y. Self-management activities in diabetes care: A systematic review. Australian Health Review 2013;37:513–22. ![]()
12. Hinder S, Greenhalgh T. “This does my head in”: Ethnographic study of self-management by people with diabetes. BMC Health Services Research, 2012; 12(83). Retrieved from http://www.biomedcentral.com/1472-6963/12/83
13. Steed L, Barnard M, Hurel S, Jenkins C, Newman S. How does change occur following a theoretically based self-management intervention for type 2 diabetes. Psychology. Health & Medicine 2014;19:536–46. ![]()
14. Wilkinson A, Whitehead L, Ritchie L. Factors influencing the ability to self-manage diabetes for adults living with type 1 or 2 diabetes. International Journal of Nursing Studies 2014;51:111–22. ![]()
15. Minet L, Lønvig E, Henriksen J, Wagner L. The experience of living with diabetes following a self-management program based on motivational interviewing. Qualitative Health Research 2011;21:1115–26. ![]()
16. van Vugt M, de Wit M, Cleijne HJJW, Snoek JF. Use of Behavioral Change Techniques in Web-Based Self-Management Programs for Type 2 Diabetes Patients: Systematic Review. J Med Internet Res. 2013;15(12):e279. ![]()
17. Webb LT, Joseph J, Yardley L, Michie S. Using the Internet to Promote Health Behavior Change: A Systematic Review and Meta-analysis of the Impact of Theoretical Basis, Use of Behavior Change Techniques, and Mode of Delivery on Efficacy. J Med Internet Res. 2010;12(1):e4. ![]()
18. Li J, Wilson LS. Telehealth Trends and the Challenge for Infrastructure. Telemedicine and E-Health. 2013;19(10):772–9. ![]()
19. El-Gayar O, Timsina P, Nawar N, Eid W. A systematic review of IT for diabetes self-management: Are we there yet? International Journal of Medical Informatics. 2013;82(8):637–52. ![]()
20. Burford S, Park S. The impact of mobile tablet devices on human information behaviour. Journal of Documentation 2014;70:622–39. ![]()
21. Orlikowski WJ. Using technology and constituting structures. Organization Science. 2000;11(4):404–28. ![]()
22. Nilsen W, Kumar S, Shar A, Varoquiers C, Wiley T, Riley WT, et al. Advancing the Science of mHealth. Journal of Health Communication. 2012;17(sup1):5–10. ![]()
23. Flanagan TR. Scripting a Collaborative Narrative: An Approach for Spanning Boundaries. Design Management Review. 2008;Summer:82–29. ![]()
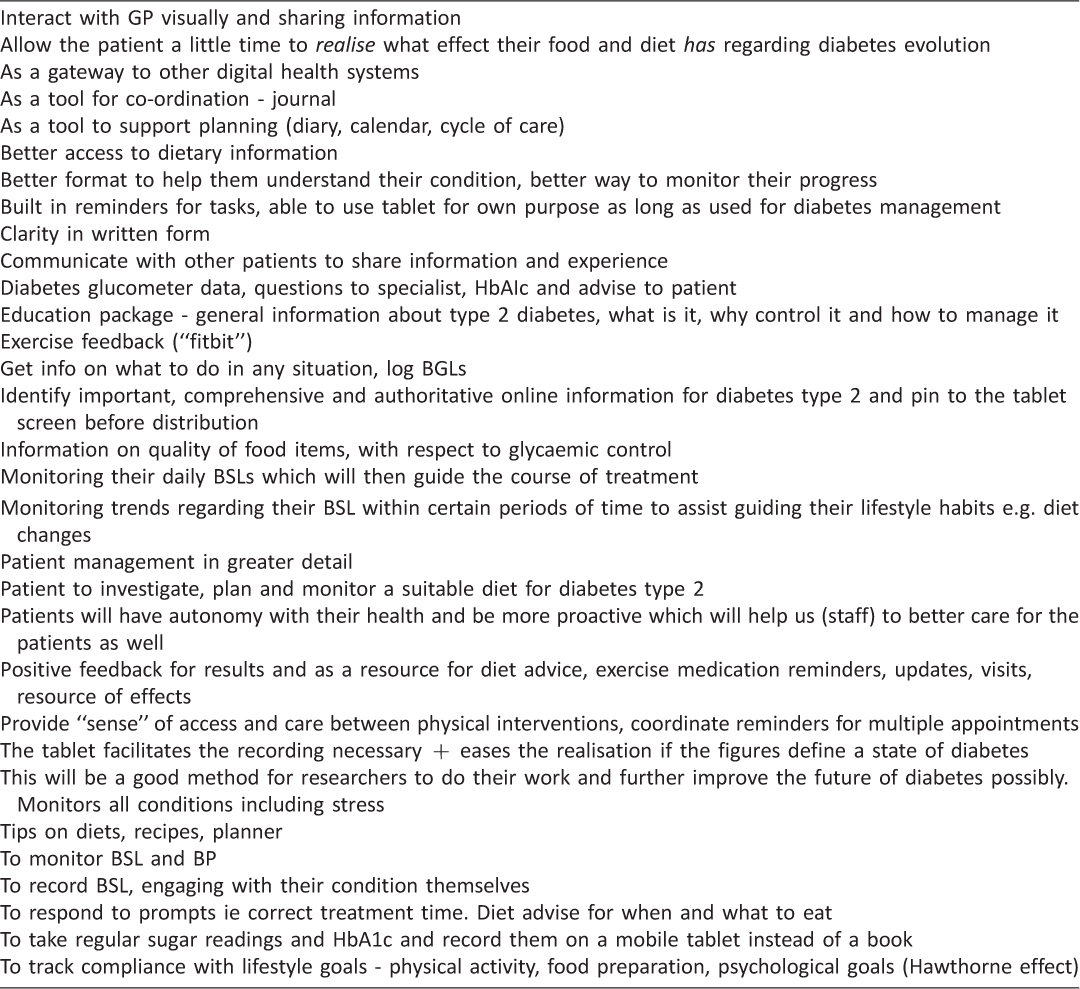
Appendix 1: List of statements
#GP Super Clinic is an initiative of Australia’s Department of Health and is a government funded program intended to bring together general practitioners, practice nurses, allied health professionals, visiting medical specialists and other health care providers to deliver primary health care services, with a patient-centric model of health care delivery.

