Published online May 18, 2016. doi: 10.5312/wjo.v7.i5.301
Peer-review started: December 9, 2015
First decision: January 4, 2016
Revised: February 2, 2016
Accepted: February 23, 2016
Article in press: February 24, 2016
Published online: May 18, 2016
Nonunion neck of femur can be a difficult problem to treat, particularly in the young, and is associated with high complication rates of avascular necrosis due to the precarious blood supply and poor biomechanics. The various treatment options that have been described can be broadly divided according to the aim of improving either biology or biomechanics. Surgeries aimed at improving the biology, such as vascularized fibula grafting, have good success rates but require high levels of expertise and substantial resources. A popular surgical treatment aimed at improving the biomechanics-valgus intertrochanteric osteotomy-optimizes conditions for fracture healing by converting shear forces across the fracture site into compressive forces. Numerous variations of this surgical procedure have been developed and successfully applied in clinical practice. As a result, the proximal femoral orientation for obtaining a good functional outcome has evolved over the years, and the present concept of altering the proximal femoral anatomy as little as possible has arisen. This technical objective supports attaining union as well as a good functional outcome, since excessive valgus can lead to increased joint reaction forces. This review summarizes the historical and current literature on valgus intertrochanteric osteotomy treatment of nonunion neck of femur, with a focus on factors predictive of good functional outcome and potential pitfalls to be avoided as well as controversies surrounding this procedure.
Core tip: Valgus intertrochanteric osteotomy is a viable treatment option for nonunion neck of femur. Size of the proximal fragment appears to be a significant predictive factor of fracture union. While valgus orientation of the proximal femur is important for fracture union, excessive valgus can lead to a poor functional outcome. The neck resorption ratio may be useful for measuring the proximal fragment and the head shaft angle may be useful for studying proximal femoral alignment in the presence of neck resorption.
- Citation: Varghese VD, Livingston A, Boopalan PR, Jepegnanam TS. Valgus osteotomy for nonunion and neglected neck of femur fractures. World J Orthop 2016; 7(5): 301-307
- URL: https://www.wjgnet.com/2218-5836/full/v7/i5/301.htm
- DOI: https://dx.doi.org/10.5312/wjo.v7.i5.301
Nonunion neck of femur (NOF) fracture remains a significant challenge to treating orthopedists in the 21st century. Indeed, some studies have shown the nonunion rate to be as high as 30%[1-3]. Nonunion following surgical fixation can result from initial fracture displacement, poor fracture reduction, or fixation in fractures with posterior comminution[4-6]. Neglected NOF fractures are more commonly seen in the developing world[7] and are associated with a particular profile of complications that includes osteopenia, resorption of neck, and avascular necrosis (AVN)[4-6]; unfortunately, these complications are also further detrimental to head salvage. The methods of treating nonunion aim either at improving the biology and bone stock (i.e., non vascularized and vascularized bone grafts[7,8], muscle pedicle graft)[9] or improving the biomechanics (i.e., valgus osteotomy)[10,11].
The concept of valgus osteotomy was refined by Pauwels[6] in 1927, according to his findings showing that nonunion NOF was due to the high shear forces that increased with the vertical orientation of the fracture. The proposed biomechanical solution was to redirect these forces into compression forces via an angulation osteotomy and fixation with a blade plate device. Valgus intertrochanteric osteotomy as described by Pauwels[6] and subsequently modified by Muller[12] is still in use today, and remains a popular treatment option as it has a high success rate and corrects the common symptoms of coxa vara and associated limb length discrepancy[11-14]. Marti et al[10] helped to popularize the valgus intertrochanteric osteotomy for nonunion NOF by reporting good outcome in a long-term follow-up study.
This review provides a summary of the historical and most up-to-date literature on the valgus intertrochanteric osteotomy for nonunion NOF, detailing the underlying philosophy and technical principles of the procedure and discussing its most common and potential complications, with the aim of helping practicing orthopedists to understand the most relevant concepts that may improve rates of good functional outcome.
The operative procedure is a modification of the method described by Muller[12].
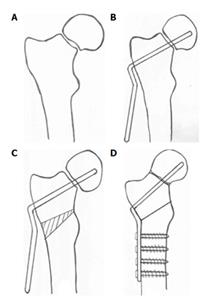
Templating, performed on the normal hip, provides information for the position of the implant and size of the wedge (Figure 1A). The angle that the fracture line makes with the horizontal should be measured. The angle of wedge measured for removal in the intertrochanteric region is necessary to ensure the vertical fracture plane achieves a near-physiological orientation. However, this angle may be difficult to calculate in patients with long-standing nonunion and can only be confirmed when a closed reduction is obtained on the fracture table[14]. Another complicating factor is that the neck in these patients is often resorbed on the inferior and posterior aspect, which can cause retroversion when impacting the fracture during fixation.
Closed reduction in case of nonunion or neglected fracture would be difficult and should be attempted on the fracture table. Excessive traction to attempt a closed reduction should be avoided as this may stretch and injure the retinaculum, which is less mobile because of surrounding scar tissue. In our experience, the proximal fragment will occasionally have an inferior spike that prevents reduction and requires osteotomization to achieve acceptable alignment. Open reduction should be attempted only if deemed essential as further dissection could damage the precarious blood supply to the femoral head. Once the reduction is maintained with K-wire, the fracture is stabilized with a screw plate or a blade plate device (Figure 1B).
A lateral closing wedge is taken from the intertrochanteric region, after which the osteotomy is closed by clamping the plate to the bone. While the calculated wedge may be as high as 40 degrees, most authors in the recent literature have reported that a wedge of 25-30 degrees is often sufficient to produce the desired effect[11,14,15]. Even in cases where an osteotomy is not required to obtain a valgus orientation, its advisable to do so as, this may help improve the blood supply to the femoral head. Compression across the fracture site can be achieved with a sliding hip screw, according to the intrinsic nature of the screw itself. However, when a double-angled blade plate device is applied, it is recommended that the length of the blade be 5-10 mm shorter than the measurement value. Firm impaction when inserting the blade plate helps to ensure that compression is obtained across the fracture site (Figure 1C and D). It is our opinion that this impaction is the most important factor in attaining union.
Often the calculated angle to convert a Pauwels 3 to Pauwels 1 may be as high as 40-50 degrees. Removal of such a large wedge will cause the osteotomy to inevitably extend from the intertrochanteric region into the subtrochanteric, which may cause further distortion of the femoral anatomy and abduction as well as external rotation deformity[16]. In addition, valgus of > 30 degrees can compromise the blood supply and increase the risk of AVN[17]. Excessive valgus could also make a salvage total hip replacement extremely difficult.
These features complicate application of the fixation device, as they may not provide enough hold. Cases with these features should be treated with a replacement rather than a fixative device.
A too long blade length may hold the fracture site in distraction, while a too short blade length may not provide adequate hold in the proximal fragment. The 110 degree and 120 degree AO double angled blade plate is available at lengths of 65, 75 and 85 mm sizes. These lengths are sufficient for most patients. However it is our practice to keep an additional set of blade plates by cutting the blades in a lathe so that blade lengths of 55 mm upwards are available in 5 mm increments. This would take care of the occasional case where it maybe required. The correct blade length cannot be over emphasized as in our opinion the impaction obtained is the single most factor to achieve union.
Previous fixation devices can create bone defects in the femoral head. Position of the blade plate in the head should be therefore in the strongest portion of the bone. Care should be taken to be not too superior or anterior, in the femoral head as this can lead to a potential cutout.
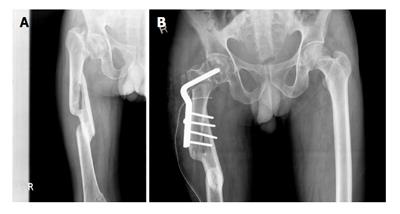
The advantages of valgus osteotomy are manifold and include preserving bone stock and avoiding total hip arthroplasty (THA) in young patients. THA in young patients is associated with higher complication rates, such as prosthesis loosening and infection, as well as higher revision rates[18]. Though recent studies have shown increased survival rates in the young[19], head salvage remains the preferable treatment, especially in a patient population which routinely sits cross-legged or squats. Therefore, while THA is the option of choice in patients who are physiologically older, head salvage via a valgus osteotomy is preferred for the younger patient population (Figure 2).
When performing an uncemented hip arthroplasty for a failed valgus osteotomy, care should be taken with the entry point so as to avoid reaming a false passage. While broaching care should be taken to negotiate over the tracts cut by the previous implants where a bridge of bone tends to form. An uncemented stem should have a distal fit and extend distal to the previous screw holes. The trochanteric fragment may remain as a nonunion and may have to be separately reattached to the femur. If the proximal femoral anatomy is grossly altered, due to a subtrochanteric osteotomy, a corrective osteotomy may be required. When there is a defect of the posteromedial cortex, use of special modular or calcar replacing stems may be required[20].
If cemented arthroplasty is performed instead, care should be taken during cementation to pressurise the screw holes externally, as the cement can track out and cause devascularisation of the sandwiched bone. It is important to note that cemented THA has been shown to be successful in revising a failed valgus osteotomy. However they have been shown to have increased complication rates in terms of survival and infection rates as compared to primary total hip replacements[21,22].
Though the presence of radiological AVN preoperatively is not a contraindication for head salvage, the reported post-valgus osteotomy AVN rates range from 10% to 40%[10,14,23]. Not all patients who develop AVN are symptomatic, and conversion rates to THA for treating post-valgus osteotomy AVN range from 5% to 10%[10,14]. For patients with the aim of hip salvage, assessing the vascularity of the head may only be of academic value. However, a report of a small series of patients with nonunion and documented AVN who underwent valgus osteotomy with vascularized fibular graft demonstrated that arrest of AVN was achieved in 3 out of the 5 patients[24].
Femoral neck shortening has been reported as associated with a poorer functional outcome in cases of acute NOF fractures[25]. As most nonunion NOF have resorbed necks, this may be a predictive factor for outcome; however, no such correlation has been shown in a series reported recently[14]. The intrinsic problem of nonunion femoral neck is the shortened neck fragment and, therefore, other options of head salvage, which can reconstruct the femoral neck length, may be effective[8,26].
The 110 and 120 degree angled blade plate, the 95 degree angled blade plate, a bent 95 degree blade plate, the sliding hip screw device, and a modified prebent dynamic condylar screw device have all been used as fixation devices for this surgery[13,27-29]. However, surgeon’s preference of implant remains largely subjective, as very little to no evidence from comparative, systematic analyses has been reported in the literature. Thus, the choice of implant may be based on the surgeon’s familiarity, as long as the principles of implantation are adhered to.
Most studies reporting valgus osteotomy emphasize union rates (Table 1) but are hampered by a lack of long-term follow-up and less than optimal functional outcome. Valgus intertrochanteric osteotomy primarily aims to convert shear forces. Earlier studies attempted to convert a Pauwels 3 to a Pauwels 1 and attained union but with excessive valgus.
| Ref. | n | Average follow-up (yr) | Union rate, n/total (%) | AVN, n/total (%) | Implant | Functional outcome |
| Marti et al[10] | 50 | 7.1 | 43/50 (86) | 22/50 (44) | DABP | HHS: 91 |
| Anglen et al[15] | 13 | 2 | 13/13 (100) | 2/13 (15) | DABP | HHS: 93 |
| Wu et al[33] | 32 | 32/32 (100) | 2/32 (6) | SHS +/- (subtrochanteric osteotomy) | NA | |
| Kalra et al[23] (neglected fractures) | 22 | 2.5 | 20/22 (85) | 2/22 (9) | DABP | 75%; excellent to good results |
| Sringari et al[34] | 20 | 2 | 18/20 (90) | Nil | DABP | NA |
| Magu et al[11] | 48 | 6 | 44/48 (94) | 2/48 (4) | DABP | HHS: 86.7 |
| Khan et al[35] | 16 | 2.5 | 14/16 (87) | Nil | SHS (120 degree plate) | HHS: 88 |
| Said et al[29] | 36 | 3.5 | 35/36 (97) | 5/36 (13) | Angled blade plate (prebent 130 degree) | NA |
| Sen et al[26] | 22 | 3.2 | 21/22 (91) | 5/55 (22) | DABP + non-vasc fibula | 66%; excellent to good results |
| Gadegone et al[7] | 41 | 2.75 | 39/41 (95) | 7/41 (17) | SHS (110-130 prebent plate + non-vasc fibula) | HHS: 90.9 |
| Gavaskar et al[28] | 11 | 1 | 11/11 (100) | Nil | SHS + subtrochanteric osteotomy, no wedge taken | Oxford score: 40 |
| Gupta et al[36] | 60 | 3.5 | 56/60 (93) | 4/60 (6) | SHS (135 degree subtrochanteric osteotomy) | HHS: 87.5 |
| Varghese et al[14] | 32 | 5 | 29/32 (91) | 13/32 (44) | DABP | HHS: 82 |
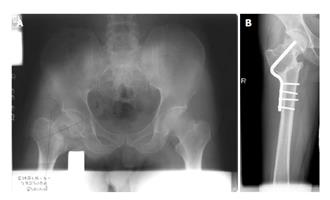
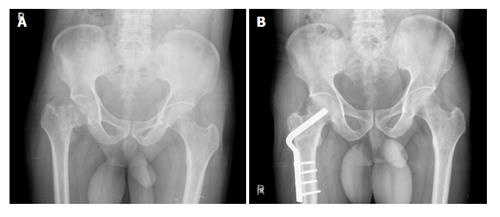
Marti et al[10] and Raaymakers et al[27] have shown that excessive valgus is detrimental to function (Figure 3). A more recent study showed that > 15 degrees of excess valgus, compared to the normal hip, results in poorer functional outcome[14]. Thus, the philosophy has evolved over the years to promoting the reproduction of as normal a proximal femoral anatomy as possible (Figure 4). Imaging and radiographic analyses are complicated in cases presenting neck resorption; the recently-described head shaft angle measurement could be a useful tool for analyzing postoperative radiographs and prognosticating functional outcome.
It would be preferable to have clear indications and contraindications for attempting head salvage in patients with femoral neck nonunion. When considering union treatment, the size of the proximal fragment seems to be an important factor. However, measurement of the proximal fragment is a complicated issue. Sandhu et al[30] reported a study in which the patients were graded according to sizes of the proximal fragment and fracture gap; it was found that patients with a head size of < 2.5 cm had the worst outcome. This classification system has its own drawbacks[11]. Magu et al[31] showed that the absolute head volume size of 43 mm3 or less, as measured by computed tomography scan, is associated with higher failure rates; however, the average volume of females in that series was 40.8 mm3, emphasizing the need for further studies in this area.
As femoral head size varies with patient height, sex and ethnicity, a ratio may be a better index than absolute size. Hence, a simple radiographic measurement called the neck resorption ratio (NRR) may be useful[14]. The NRR is a measure of the remnant of the femoral head to the neck length on the sound side, and thus does not vary with traction or magnification of the plate X-ray and can be read on a simple anteroposterior pelvis radiograph. The three nonunion cases, which occurred in this study, were included in the group with an NRR of < 0.5. Thus, head salvage would be indicated in a physiologically young, active patient with sufficient bone stock and would be contraindicated in an older patient with an NRR of < 0.5.
There is a significant percentage of nonunion NOF in the young. Moreover in developing countries there is an additional problem of neglected fractures[32]. It would appear that nonunions are increasingly being treated with arthroplasty, even in the young, with an additional need for revision. In this group of patients the valgus osteotomy would remain a viable alternative, especially in places where social and religious activities require squatting and sitting cross legged. Valgus osteotomy remains a successful method of head salvage in cases of nonunion and neglected NOF fractures. Excessive valgus may impair the final functional outcome; in cases presenting with resorbed neck (> 50%), arthroplasty would be a better option.
P- Reviewer: Aprato A, Carbone S S- Editor: Ji FF L- Editor: A E- Editor: Liu SQ
| 1. | Mathews V, Cabanela ME. Femoral neck nonunion treatment. Clin Orthop Relat Res. 2004;57-64. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 46] [Cited by in F6Publishing: 44] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 2. | Lu-Yao GL, Keller RB, Littenberg B, Wennberg JE. Outcomes after displaced fractures of the femoral neck. A meta-analysis of one hundred and six published reports. J Bone Joint Surg Am. 1994;76:15-25. [PubMed] [Cited in This Article: ] |
| 3. | Damany DS, Parker MJ, Chojnowski A. Complications after intracapsular hip fractures in young adults. A meta-analysis of 18 published studies involving 564 fractures. Injury. 2005;36:131-141. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 16] [Cited by in F6Publishing: 49] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 4. | Parker MJ. Prediction of fracture union after internal fixation of intracapsular femoral neck fractures. Injury. 1994;25 Suppl 2:B3-B6. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 7] [Article Influence: 0.2] [Reference Citation Analysis (1)] |
| 5. | Haidukewych GJ, Berry DJ. Salvage of failed treatment of hip fractures. J Am Acad Orthop Surg. 2005;13:101-109. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 43] [Cited by in F6Publishing: 37] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 6. | Pauwels F. Biomechanics of the normal and diseased hip. 1976;. [DOI] [Cited in This Article: ] |
| 7. | Gadegone WM, Ramteke AA, Lokhande V, Salphade Y. Valgus intertrochanteric osteotomy and fibular strut graft in the management of neglected femoral neck fracture. Injury. 2013;44:763-768. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 17] [Cited by in F6Publishing: 16] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 8. | LeCroy CM, Rizzo M, Gunneson EE, Urbaniak JR. Free vascularized fibular bone grafting in the management of femoral neck nonunion in patients younger than fifty years. J Orthop Trauma. 2002;16:464-472. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 72] [Cited by in F6Publishing: 70] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 9. | Meyers MH, Harvey JP, Moore TM. Delayed treatment of subcapital and transcervical fractures of the neck of the femur with internal fixation and a muscle pedicle bone graft. Orthop Clin North Am. 1974;5:743-756. [PubMed] [Cited in This Article: ] |
| 10. | Marti RK, Schüller HM, Raaymakers EL. Intertrochanteric osteotomy for non-union of the femoral neck. J Bone Joint Surg Br. 1989;71:782-787. [PubMed] [Cited in This Article: ] |
| 11. | Magu NK, Rohilla R, Singh R, Tater R. Modified Pauwels’ intertrochanteric osteotomy in neglected femoral neck fracture. Clin Orthop Relat Res. 2009;467:1064-1073. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 28] [Cited by in F6Publishing: 32] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 12. | Muller ME. Intertrochanteric osteotomy: indications, preoperative planning, technique. Berlin: Springer-Verlag 1984; 25-66. [DOI] [Cited in This Article: ] |
| 13. | Deakin DE, Guy P, O’Brien PJ, Blachut PA, Lefaivre KA. Managing failed fixation: valgus osteotomy for femoral neck nonunion. Injury. 2015;46:492-496. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 15] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 14. | Varghese VD, Boopalan PR, Titus VT, Oommen AT, Jepegnanam TS. Indices affecting outcome of neglected femoral neck fractures after valgus intertrochanteric osteotomy. J Orthop Trauma. 2014;28:410-416. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 24] [Cited by in F6Publishing: 19] [Article Influence: 1.9] [Reference Citation Analysis (1)] |
| 15. | Anglen JO. Intertrochanteric osteotomy for failed internal fixation of femoral neck fracture. Clin Orthop Relat Res. 1997;175-182. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 47] [Cited by in F6Publishing: 33] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 16. | Magu NK, Singh R, Mittal R, Garg R, Wokhlu A, Sharma AK. Osteosynthesis and primary valgus intertrochanteric osteotomy in displaced intracapsular fracture neck of femur with osteoporosis in adults. Injury. 2005;36:110-122. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 26] [Cited by in F6Publishing: 27] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 17. | Calandruccio RA, Anderson WE. Post-fracture avascular necrosis of the femoral head: correlation of experimental and clinical studies. Clin Orthop Relat Res. 1980;49-84. [PubMed] [Cited in This Article: ] |
| 18. | Gililland JM, Anderson LA, Erickson J, Pelt CE, Peters CL. Mean 5-year clinical and radiographic outcomes of cementless total hip arthroplasty in patients under the age of 30. Biomed Res Int. 2013;2013:649506. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 20] [Cited by in F6Publishing: 20] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 19. | Wroblewski BM, Siney PD, Fleming PA. Charnley low-frictional torque arthroplasty: follow-up for 30 to 40 years. J Bone Joint Surg Br. 2009;91:447-450. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 62] [Cited by in F6Publishing: 65] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 20. | Haidukewych GJ, Berry DJ. Hip arthroplasty for salvage of failed treatment of intertrochanteric hip fractures. J Bone Joint Surg Am. 2003;85-A:899-904. [PubMed] [Cited in This Article: ] |
| 21. | Ferguson GM, Cabanela ME, Ilstrup DM. Total hip arthroplasty after failed intertrochanteric osteotomy. J Bone Joint Surg Br. 1994;76:252-257. [PubMed] [Cited in This Article: ] |
| 22. | Breusch SJ, Lukoschek M, Thomsen M, Mau H, Ewerbeck V, Aldinger PR. Ten-year results of uncemented hip stems for failed intertrochanteric osteotomy. Arch Orthop Trauma Surg. 2005;125:304-309. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 22] [Cited by in F6Publishing: 21] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 23. | Kalra M, Anand S. Valgus intertrochanteric osteotomy for neglected femoral neck fractures in young adults. Int Orthop. 2001;25:363-366. [PubMed] [Cited in This Article: ] |
| 24. | Beris AE, Payatakes AH, Kostopoulos VK, Korompilias AV, Mavrodontidis AN, Vekris MD, Kontogeorgakos VA, Soucacos PN. Non-union of femoral neck fractures with osteonecrosis of the femoral head: treatment with combined free vascularized fibular grafting and subtrochanteric valgus osteotomy. Orthop Clin North Am. 2004;35:335-343, ix. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 31] [Cited by in F6Publishing: 31] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 25. | Zlowodzki M, Ayeni O, Petrisor BA, Bhandari M. Femoral neck shortening after fracture fixation with multiple cancellous screws: incidence and effect on function. J Trauma. 2008;64:163-169. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 78] [Cited by in F6Publishing: 86] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 26. | Sen RK, Tripathy SK, Goyal T, Aggarwal S, Tahasildar N, Singh D, Singh AK. Osteosynthesis of femoral-neck nonunion with angle blade plate and autogenous fibular graft. Int Orthop. 2012;36:827-832. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 22] [Cited by in F6Publishing: 22] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 27. | Raaymakers EL, Marti RK. Nonunion of the femoral neck: possibilities and limitations of the various treatment modalities. Indian J Orthop. 2008;42:13-21. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 26] [Cited by in F6Publishing: 28] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 28. | Gavaskar AS, Chowdary NT. Valgus sliding subtrochanteric osteotomy for neglected fractures of the proximal femur; surgical technique and a retrospective case series. J Orthop Surg Res. 2013;8:4. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 11] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 29. | Said GZ, Farouk O, Said HG. Valgus intertrochanteric osteotomy with single-angled 130° plate fixation for fractures and non-unions of the femoral neck. Int Orthop. 2010;34:1291-1295. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 31] [Cited by in F6Publishing: 27] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 30. | Sandhu HS, Sandhu PS, Kapoor A. Neglected fractured neck of the femur: a predictive classification and treatment by osteosynthesis. Clin Orthop Relat Res. 2005;14-20. [PubMed] [Cited in This Article: ] |
| 31. | Magu NK, Magu S, Rohilla RK, Batra A, Jaipuria A, Singh A. Computed tomographic evaluation of the proximal femur: A predictive classification in displaced femoral neck fracture management. Indian J Orthop. 2014;48:476-483. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 8] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 32. | Jain AK, Mukunth R, Srivastava A. Treatment of neglected femoral neck fracture. Indian J Orthop. 2015;49:17-27. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 21] [Cited by in F6Publishing: 25] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 33. | Wu CC, Shih CH, Chen WJ, Tai CL. Treatment of femoral neck nonunions with a sliding compression screw: comparison with and without subtrochanteric valgus osteotomy. J Trauma. 1999;46:312-317. [PubMed] [Cited in This Article: ] |
| 34. | Sringari T, Jain UK, Sharma VD. Role of valgus osteotomy and fixation by double-angle blade plate in neglected displaced intracapsular fracture of neck of femur in younger patients. Injury. 2005;36:630-634. [PubMed] [Cited in This Article: ] |
| 35. | Khan AQ, Khan MS, Sherwani MK, Agarwal R. Role of valgus osteotomy and fixation with dynamic hip screw and 120 degrees double angle barrel plate in the management of neglected and ununited femoral neck fracture in young patients. J Orthop Traumatol. 2009;10:71-78. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 22] [Cited by in F6Publishing: 21] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 36. | Gupta S, Kukreja S, Singh V. Valgus osteotomy and repositioning and fixation with a dynamic hip screw and a 135º single-angled barrel plate for un-united and neglected femoral neck fractures. J Orthop Surg (Hong Kong). 2014;22:13-17. [PubMed] [Cited in This Article: ] |