Published online May 16, 2014. doi: 10.4253/wjge.v6.i5.168
Revised: April 3, 2014
Accepted: April 16, 2014
Published online: May 16, 2014
Although less common than oesophageal variceal haemorrhage, gastric variceal bleeding remains a serious complication of portal hypertension, with a high associated mortality. In this review we provide an update on the aetiology, classification and management of gastric varices, including acute bleeding, prevention of rebleeding and primary prophylaxis. We describe the optimum management strategies for gastric varices including drug, endoscopic and radiological therapies, focusing on recent published evidence.
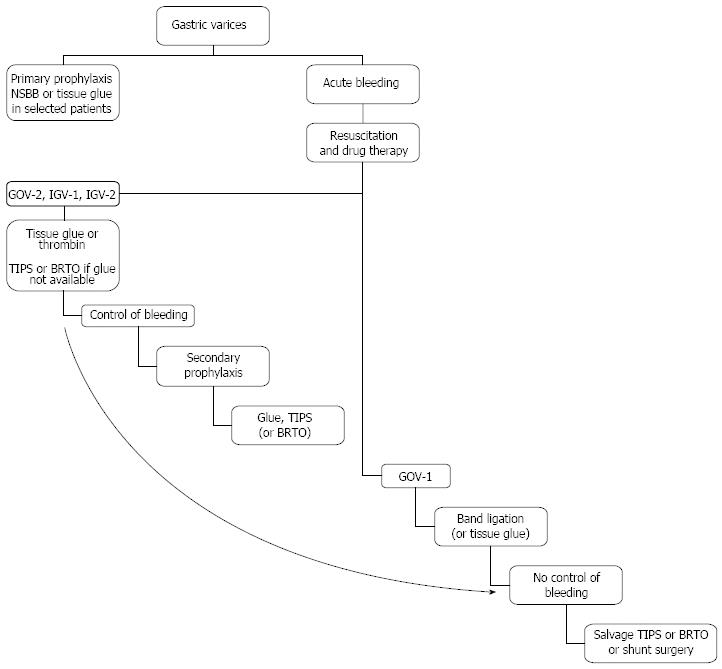
Core tip: Endoscopic injection of cyanoacrylate is currently the optimum, evidenced based approach to control active bleeding from gastric varices, apart from bleeding from gastro-oesophageal varice (GOV)-1 which can be treated with variceal band ligation. Transjugular intrahepatic portosystemic shunt (or balloon-occluded retrograde transvenous obliteration in experienced units) can be effective for ongoing bleeding. Cyanoacrylate or transjugular intrahepatic portosystemic shunt can prevent rebleeding from GOV-2 or isolated gastric varice, although variceal band ligation, cyanoacrylate or β-blockers can be used after bleeding from GOV-1. Non-selective β-blockers or cyanoacrylate may be used as primary prophylaxis in patients with known gastric varices, with the choice dependent on clinical and endoscopic findings.
- Citation: Triantafyllou M, Stanley AJ. Update on gastric varices. World J Gastrointest Endosc 2014; 6(5): 168-175
- URL: https://www.wjgnet.com/1948-5190/full/v6/i5/168.htm
- DOI: https://dx.doi.org/10.4253/wjge.v6.i5.168
Gastric varices occur in around 20% of patients with portal hypertension, mostly secondary to liver cirrhosis[1]. Although they bleed less frequently than oesophageal varices, gastric variceal bleeding tends to be more severe with a reported mortality of approximately 45%. In this review, we describe the causes, classification and management of gastric variceal bleeding.
Pathogenesis of portal hypertension can be secondary to intra-hepatic (e.g., cirrhosis, nodular regenerative hyperplasia), pre-hepatic (e.g., portal or splenic venous obstruction) or post-hepatic (e.g., hepatic venous obstruction) aetiology. Gastric varices can arise due to any of these causes of portal hypertension, but are particularly frequent in patients with splenic or portal venous obstruction.
Risk factors for gastric variceal bleeding include variceal size (large, medium and small defined as > 10 mm, 5-10 mm and < 5 mm respectively), advanced Child’s grade of cirrhosis, presence of hepatocellular carcinoma, location of gastric varices (see below) and presence of red spots[1,2].
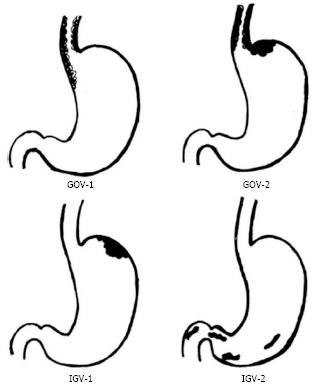
Gastric varices are most commonly described using Sarin’s classification[1]. This system uses their location in the stomach and their relationship to oesophageal varices. It divides them into gastro-oesophageal varices (GOVs) or isolated gastric varices (IGVs). GOVs are further sub-divided into GOV-1 which extend for 2-5 cm along the lesser curve of the stomach and GOV-2 which extend beyond the gastro-oesophageal junction into the fundus of the stomach. IGVs are sub-divided into IGV-1 located in the fundus and IGV-2 located in the gastric body, antrum or pylorus (Figure 1)[1,3]. Figure 2 shows an endoscopic picture of IGV-1. Hashizume and colleagues also described a classification of gastric varices including their form, location and color, although this is less commonly used[4].
Variceal haemorrhage should be suspected when a patient with known cirrhosis or evidence of portal hypertension presents with upper gastrointestinal haemorrhage. Volume restitution should be commenced immediately to maintain haemodynamic stability with blood transfusion as necessary aiming for target haemoglobin of 7-8 g/dL[5,6]. A recent Spanish randomized controlled trial showed that in Childs grade A or B cirrhotic patients with oesophageal or gastric variceal bleeding, transfusing below a threshold of 7 g/dL is safe and reduces rebleeding, need for rescue therapy and mortality[6].
Prophylactic antibiotics should be administrated early to patients with suspected or confirmed variceal bleeding as this has been shown to reduce mortality and risk of infection[7,8]. Oral quinolones are often recommended, however the antibiotic choice is often guided by local microbiological advice[5].
Vasoactive drugs should be commenced as soon as possible if variceal bleeding is suspected[5,9]. A meta-analysis comparing emergency sclerotherapy with pharmacologic treatment (including terlipressin, somatostatin or octreotide) for variceal bleeding in cirrhosis showed that vasoactive drugs are beneficial as first-line treatment[10]. However, most patients had oesophageal variceal bleeding. To date, no studies have investigated the use of vasoactive drugs specifically for gastric variceal bleeding. Early endoscopy should be undertaken to confirm the diagnosis and allow endoscopic therapy as required (see below).
Although no formal studies have assessed its use in gastric varices, the temporary use of an intra-gastric balloon such as the Sengstaken-Blackmore tube to tamponade fundal varices may be helpful if bleeding continues despite pharmacologic and endoscopic therapies. This is often used as a bridge to more definitive therapy including placement of a transjugular intrahepatic portosystemic shunt (TIPS; see below)[9,11].
Endoscopic treatment for gastric variceal bleeding includes endoscopic band ligation, sclerotherapy and endoscopic injection of tissue adhesives or thrombin.
Variceal band ligation: Variceal band ligation is the gold standard for the endoscopic management of oesophageal variceal haemorrhage[5,7], but its role in gastric variceal bleeding is less clear. In a prospective randomized trial by Tan et al[12], the efficacy of band ligation to arrest active gastric variceal bleeding in cirrhotic patients was comparable to cyanoacrylate injection, but the rebleeding rate was higher in the banding group. No difference in complications was found between the groups[12].
A study comparing variceal band ligation with the endoscopic use of detachable snares in controlling acute gastric and oesophageal variceal bleeding showed no difference between the two approaches in achieving haemostasis[13]. However variceal recurrence and rebleeding rates were relatively high in both groups. Band ligation is not covered by NICE guidelines for the management of gastric variceal bleeding. However, Baveno V and AASLD guidelines suggest this type of treatment is of particular use in the endoscopic management of bleeding GOV-1, as these are generally considered extensions of oesophageal varices[5,9]. AASLD guidelines also suggest that endoscopic variceal band ligation is an option for patients who bleed from gastric fundal varices if cyanoacrylate is not available[9]. However band ligation is not of proven efficacy for non GOV-1 gastric variceal bleeding.
Sclerotherapy: A study of gastric variceal sclerotherapy with pure alcohol for acute gastric variceal bleeding reported a haemostatic rate of 66%[3]. Gastric variceal sclerotherapy appears more effective in GOV-1 than GOV-2 or IGV-1[3]. However complications associated with the procedure include fever, retrosternal and abdominal pain, dysphagia, rebleeding and ulceration. Similar to the management of oesophageal variceal bleeding, sclerotherapy has been largely replaced by band ligation when appropriate, due to the latter’s lower complication and rebleeding rates.
Tissue glues: Cyanoacrylate is a monomer that undergoes rapid polymerization in presence of ionic substances including blood or tissue fluids. Tissue adhesives include histoacryl (N-butyl-cyanoacrylate) and bucrylate (isobutyl -2-cyanoacrylate) and both have been used with success for gastric varices obliteration. A standard forward viewing endoscope is used and the accessory channel and needle catheter are first flushed with lipiodol. The needle is then inserted into the gastric varix and a mixture of lipiodol and tissue adhesive is administered into the varix followed by a flush of saline or sterile water. The needle should be withdrawn immediately to prevent adherence to the varix, then flushed again with saline or sterile water. Injections can be repeated until obliteration of the varices is achieved. Obturation can be confirmed by palpation of the varices using the probe with the needle retracted.
Paik et al[14] retrospectively reviewed 121 patients with active or recent gastric variceal bleeding who were treated with N-butyl 2-cyanoacrylate. Bleeding control was achieved in 91% of patients with a 4-wk rebleeding rate of 13%. Fever occurred in 11% of patients and 2% had severe complications attributed to cyanoacrylate embolisms, which however resolved with conservative management. Kang et al[15] reported a 98% rate of haemostasis with histoacryl, with few complications. Similar to other studies, fever and abdominal pain were observed, but several uncommon complications were also reported including pulmonary embolism, splenic infarction and adrenal abscess. Case reports of thromboembolic episodes to the pulmonary cerebral and coronary circulation after tissue adhesive injection have also been described[16]. A United Kingdom study achieved an immediate haemostasis rate of 100% with endoscopic histoacryl injection in gastric variceal bleeding[17], and Al-Ali et al[18] reported a haemostasis rate of 95% in a Canadian population. Both studies reported no significant complications. A high haemostasis rate of 95% was also reported in a large study performed by Cheng and colleagues[19].
Current evidence of the use of tissue adhesives for gastric variceal bleeding suggests haemostasis control in > 90%. Table 1 summarizes some of the larger and most recent studies using cyanoacrylate for the treatment of gastric varices[14,15,17-21].
| Ref. | Type of study | No. of patients (follow-up) | Active bleeding | Haemostasis rate | Rebleeding rate | Complications |
| Cheng et al[19] | Case series | 613 (30 mo) | 23% | 95% | 8% | 5% “major” |
| Kang et al[15] | Retrospective | 127 (18 mo) | 38% | 98% | 23% | 3 % “major” |
| Seewaldet al[20] | Retrospective | 131 (26 mo) | 63% | 100% | 7% | 0% |
| Paik et al[14] | Retrospective | 121 (12 mo) | 26% | 91% | 13% (at 4 wk) | 2% (major complications) |
| Kind et al[21] | Case series | 174 (36 mo) | 100% | 97% | 13% “late rebleeding” | 8% |
| Ali-Al et al[18] | Retrospective | 37 (14 mo) | 86% | 95% | 28% | 0 % “major” |
| Rajoriyaet al[17] | Retrospective | 31 (35 mo) | Not recorded | 100% | 16% | 0 % “major” |
| 6% “minor” |
A randomized trial of cyanoacrylate injection vs TIPS for gastric variceal bleeding showed similar survival and complication rates in both groups, but TIPS was more effective in preventing rebleeding (11% vs 38%)[22]. Cyanoacrylate was also compared to TIPS in another two (non-randomised) studies, again with similar haemostasis rates reported between both groups[23,24].
Tissue adhesives appear to be relatively safe and effective in the management of bleeding gastric varices and are generally the endoscopic treatment of choice for bleeding from IGVs and GOV-2. They are recommended by the Baveno V, NICE and AASLD guidelines[5,7,9]. Although there are a few technical issues, appropriate training and use of a unit protocol enable most centers to use it safely and effectively.
Thrombin: Thrombin affects haemostasis by converting fibrinogen to fibrin clot and also influences platelet aggregation[25]. A standard gastroscope is used for the procedure and no specific preparation is required.
Williams et al[26] used bovine thrombin for control of gastric variceal bleeding and reported 100% haemostasis with no significant complications and a low rebleeding rate. Ramesh and colleagues also studied bovine thrombin in the management of bleeding gastric varices[27]. They reported 92% haemostasis in the acute setting, with no rebleeding during follow-up. No patient had an adverse event and no technical problems were encountered. More recent studies have used human rather than bovine thrombin because of the concerns of spongiform encephalopathy.
The largest study to evaluate the efficacy of human thrombin in the management of gastric and ectopic varices bleeding suggests that human thrombin is safe and effective[28]. Thrombin is a promising therapy for bleeding gastric varices but to date no randomized data on its use are available and longer term follow-up is required, therefore more studies are required. Table 2 summarizes some of the largest and more recent studies reporting thrombin use in gastric variceal bleeding[26-29].
Radiologic therapies for gastric varices include TIPS and BRTO (balloon-occluded retrograde transvenous obliteration).
TIPS: TIPS has been well studied in the management of oesophageal varices, with fewer studies undertaken on its use in bleeding gastric varices. An American retrospective comparative study compared TIPS with cyanoacrylate injection for gastric variceal bleeding. No differences were found in survival or rebleeding, but the group treated with TIPS had an increased morbidity requiring prolonged hospitalization because of encephalopathy[23].
Another study compared the clinical outcome of PTFE-coated stent-grafts with bare stents in patients who required emergency or elective TIPS for portal hypertension related complications[30]. During follow-up, 22% of the patients with bare stents had clinically relevant TIPS dysfunction, but no dysfunction was observed in patients treated with coated stent-grafts. Encephalopathy rates were similar. TIPS can also be used if bleeding from gastric varices is not controlled with N-butyl-cyanoacrylate injection, however the portal vein must be patent and careful patient selection is required to minimize risks of encephalopathy[7,31].
Balloon-occluded retrograde transvenous obliteration: Balloon-occluded retrograde transvenous obliteration (BRTO) is a radiologic technique used for the treatment of gastric varices. The right femoral or internal jugular vein is punctured and a balloon catheter is inserted into the left renal vein. After balloon inflation, venography is performed to identify gastric varices, gastrorenal shunts and collateral veins. The veins draining gastric varices are embolised with microcoils and a sclerosant agent is injected until all varices are obliterated.
Hong et al[32] compared BRTO with endoscopic injection of cyanoacrylate in the management of acute gastric variceal bleeding and high risk varices (≥ 5 mm with red spots and Child’s grade B or C). The haemostasis and rebleeding rates of cyanoacrylate were 100% and 71.4% respectively compared with 76.9% and 15.4% respectively for BRTO. This was a surprising high rate of rebleeding after cyanoacrylate treatment, but included a higher proportion of patients with active bleeding than most studies. Complications were similar. The patients who rebelled were treated with rescue cyanoacrylate or BRTO. These results suggest that BRTO may have a role as rescue therapy in patients with gastric variceal bleeding.
In a small randomized study performed by Choi et al[33], BRTO was compared with TIPS for the urgent treatment of active gastric variceal haemorrhage. No differences were found between the groups in immediate haemostasis, rebleeding or encephalopathy. BRTO can be an alternative to TIPS for the management of acute gastric variceal bleeding if gastro-renal shunts are present[33]. However it is rarely performed outside Asian centers[34]. None of AASLD, NICE or Baveno V guidelines specifically recommend BRTO as treatment for gastric varices.
Therapeutic options for the prevention of gastric variceal rebleeding include use of non-selective β-blockers, repeated endoscopic injection of tissue adhesives, endoscopic band ligation (TIPS, BRTO), surgical intervention and liver transplantation.
A randomized controlled trial compared endoscopic cyanoacrylate injection with non-selective β-blockers in the secondary prevention of gastric variceal bleeding[35]. Patients with GOV-2 or IGV-1 were included and HVPG measurement was undertaken to assess the response to β-blockade. The cumulative two year survival rates in the cyanoacrylate and β-blocker groups were 90% and 52% respectively, with the difference linked to higher rebleeding in the β-blocker group. The median HVPG in the group treated with β-blockers fell on follow-up but rose in the cyanoacrylate group, which may be attributed to redistribution of blood flow in the portal system after variceal obturation. There was no difference in complication rates.
Another recent randomized controlled trial was reported by Hung et al[36] compared repeated gastric variceal obturation with or without non-selective β-blockers in patients with bleeding GOV-2 and IGV-1. The overall mortality and rebleeding rates during follow-up were similar in the two groups although adverse effects were more common in the combination group. Therefore combining non-selective β-blockers with gastric variceal obturation does not appear to have a role in preventing GOV-2 or IGV-1 rebleeding. However the use of non-selective β-blockers may have a role in GOV-1, similar to the management of oesophageal varices[5].
Variceal banding: Due to the issues described above, variceal banding is generally only used as secondary prophylaxis for GOV-1 varices, but not for other types of gastric varices.
Tissue adhesives: As noted above, cyanoacrylate injection is significantly more effective than β-blocker treatment for the prevention of rebleeding from gastric varices[35] and has a lower rebleeding rate compared with band ligation in this situation[12]. As stated above, in a randomized study, rebleeding was higher in patients treated with cyanoacrylate compared with TIPS[22]. However both therapies have similar survival, and there are fewer complications with cyanoacrylate which also appears more cost-effective[22-24].
The United Kingdom study reporting long-term results of endoscopic histoacryl injection in gastric variceal bleeding reported a rebleeding rate of 16%. The mean overall follow-up was 35 mo[17]. The Canadian study, with a median follow-up period of 14 mo, reported a late rebleeding rate of 28%[18]. During a follow-up period of 30 mo, 8% of the patients in Cheng’s study had recurrent bleeding[19].
Current evidence on the use of tissue adhesives for gastric variceal bleeding report re-bleeding rates of 7%-38%, with relatively few complications (Table 1).
Thrombin: Thrombin seems to be an effective and safe treatment to reduce gastric variceal rebleeding and repeated injections to achieve eradication may not be necessary[25-29]. Reported rates of rebleeding vary from 0-27% (Table 2)[26-29]. As indicated above, more studies are needed to provide comparative data with other treatment modalities before thrombin injection can be routinely used for prevention of gastric variceal rebleeding.
TIPS: Tripathi described TIPS placement in 40 patients with gastric variceal bleeding, 232 with oesophageal, 12 with oesophageal and gastric and 8 with ectopic variceal bleeding[37]. All of the patients had portal hypertension due to parenchymal liver disease. The portal pressure gradient (PPG) before TIPS was lower in the patients with gastric variceal bleeding. Fourteen point seven percent of the patients with oesophageal varices and 20% with gastric varices rebled. Complication rates were similar. Mortality was lower in patients with gastric varices, but only if pre-TIPS PPG was ≥ 12 mmHg. Most patients who bled after TIPS had a PPG > 7 mmHg suggesting this may be the target to protect against gastric variceal rebleeding. TIPS insertion appears effective for the prevention of gastric variceal rebleeding, although it is more invasive than endoscopic methods, has associated risks of encephalopathy and is not always available[22,30,37].
BRTO: A retrospective study performed by Jang evaluated the clinical outcomes of BRTO for the management of gastric variceal hemorrhage[38]. In 183 patents with confirmed gastric variceal bleeding, BRTO was performed with a technical success of 96.7%, and procedure-related complications occurred in 4.4%. Overall rebleeding rate was 22%.
Cho[39] evaluated clinical outcomes of BRTO in 49 patients who had gastric varices with spontaneous gastro-systemic shunts. Procedural success rate was 83.7% but there were two procedure-related deaths. Other complications included fever, ascites, pleural effusion, portal vein thrombosis, pulmonary thromboembolism and hemoglobinuria. No variceal recurrence or rebleedingwas noted. BRTO can increase PPG, secondary to increased hepato-portal flow and may aggravate pre-existing oesophageal varices and ascites[39,40]. However BRTO is a procedure that preserves hepatic function and can be used in patients with gastric varices and gastrorenal shunts if TIPS is not possible[34].
The Hong Kong group suggested that patients who undergo EUS-guided cyanoacrylate injection have a significantly lower risk of recurrent bleeding from gastric varices during subsequent follow-up[41]. However others have not confirmed this[17]. There may be a role for ultrasound mini-probes in the future to assess variceal obliteration, but at present this remains an investigative technique.
A new method has been reported for the management of gastric varices with EUS which is a combination of 2-octyl-cyanoacrylate and coils[42]. Thirty patients with acute or recent bleeding from GOV-2 and IGV-1 were treated and use of coils seemed to retain cyanoacrylate with a lower volume required to obliterate varices. Haemostasis was achieved in 100% of patients with a 96% variceal obliteration rate and no procedure related complications. More studies are needed to determine the efficacy of this treatment.
Surgical therapies include total shunts, partial (lower diameter) shunts, selective shunts and devascularization procedures. Total shunts control and prevent variceal bleeding but do not improve survival and often precipitate encephalopathy. Selective shunts have lower rates of encephalopathy and are more commonly used[43]. Eighty percent of patients have good control of bleeding and maintenance of portal perfusion with a selective distal splenorenal shunt[44]. Orloff reported that a portal-systemic shunt can be an effective therapy for bleeding varices in patients with portal vein thrombosis and preserved liver function[45]. They reported no recurrent bleeding or encephalopathy and good survival rates. Splenectomy may have a role if there are IGV-1 secondary to an isolated splenic vein thrombosis[9].
Surgery for portal hypertension should be performed by experienced surgeons, in lower risk patients[43]. It is generally considered as rescue therapy, due to the associated risks and the increasing use of simpler endoscopic and radiologic procedures as described above. Liver transplantation should also be considered for eligible patients.
The Baveno V guidelines suggest use of cyanoacrylate or TIPS for the prevention of rebleeding in patients with IGV-1 and GOV-2. The AASLD guidelines consider TIPS as a treatment in patients with recurrent bleeding from fundal varices despite pharmacological and endoscopic therapy.
A recent randomized study compared the efficacy of β-blockers, cyanoacrylate injection and no active treatment in the primary prevention of GOV-2 and IGV-1 gastric variceal bleeding[46]. Thirty eight percent, 10% and 53% of the patients bled in the β-blocker, cyanoacrylate and no-treatment groups respectively, over a median follow-up period of 26 mo. The cyanoacrylate group had significantly lower bleeding rates than the other groups for GOV-2, but not for IGV-1 patients. Mortality was significantly lower in the group treated with cyanoacrylate (7%) compared with those given no-treatment (26%) but was not significant compared with the β-blockers group (17%). β-blockers, even if HPVG fell, did not reduce the incidence of first bleeding or mortality. Therefore other factors including high variceal flow or size of gastric varices may be responsible for bleeding.
Kang et al[15] retrospectively analyzed patients with cirrhosis and suggested that cyanoacrylate injection is a valuable treatment for gastric varices and also an effective prophylactic treatment for high risk gastric varices.
A retrospective study by Katoh et al[47] evaluated the clinical outcomes of BRTO for the treatment of gastric varices. Forty-seven patients were included and it was performed as a primary prophylactic treatment in 40 patients[47]. Technique was successful in 79% with 1 and 5 year survival of 92% and 73% respectively. However this procedure is rarely performed outside Asia. Whilst relatively invasive endoscopic and radiologic procedures may have a future role in the primary prophylaxis of gastric variceal bleeding, more comparative studies are needed.
Despite the paucity of high quality studies assessing primary prophylactic therapy for gastric variceal bleeding, the Baveno V guidelines recommended that patients with gastric varices may be treated with non-selective β-blockers[5]. However these guidelines were published prior to the Indian RCT which suggested a role for cyanoacrylate in this situation[46]. The choice of therapy in this situation may well depend on variceal size, underlying liver function and other clinical factors.
Gastric variceal bleeding is a medical emergency with a high mortality. There are relatively few randomized studies assessing management of this condition, therefore guidance on therapy is based on relatively low quality data. However endoscopic injection of tissue glue or thrombin, appear effective in control of bleeding, with TIPS (or BRTO) an option if bleeding continues. To prevent rebleeding from IGV or GOV-2, cyanoacrylate or TIPS is recommended and after bleeding from GOV-1, band ligation, cyanoacrylate, or β-blockers may be used. For primary prophylaxis, patients with gastric varices may be treated with non-selective β-blockers, or possibly cyanoacrylate in selected cases. However further high quality studies are required to help clarify therapeutic strategies in this condition.
A suggested algorithm for the management of gastric varices is shown in Figure 3.
Dr. Maria Triantafyllou, co-authored this article while she had an attachment in Glasgow Royal Infirmary, which was supported by the Hellenic Society of Gastroenterology and Nutrition (ELIGAST).
P- Reviewer: Yeh HZ S- Editor: Song XX L- Editor: A E- Editor: Zhang DN
| 1. | Sarin SK, Lahoti D, Saxena SP, Murthy NS, Makwana UK. Prevalence, classification and natural history of gastric varices: a long-term follow-up study in 568 portal hypertension patients. Hepatology. 1992;16:1343-1349. [Cited in This Article: ] |
| 2. | Kim T, Shijo H, Kokawa H, Tokumitsu H, Kubara K, Ota K, Akiyoshi N, Iida T, Yokoyama M, Okumura M. Risk factors for hemorrhage from gastric fundal varices. Hepatology. 1997;25:307-312. [Cited in This Article: ] |
| 3. | Sarin SK. Long-term follow-up of gastric variceal sclerotherapy: an eleven-year experience. Gastrointest Endosc. 1997;46:8-14. [Cited in This Article: ] |
| 4. | Hashizume M, Kitano S, Yamaga H, Koyanagi N, Sugimachi K. Endoscopic classification of gastric varices. Gastrointest Endosc. 1990;36:276-280. [Cited in This Article: ] |
| 5. | de Franchis R. Revising consensus in portal hypertension: report of the Baveno V consensus workshop on methodology of diagnosis and therapy in portal hypertension. J Hepatol. 2010;53:762-768. [Cited in This Article: ] |
| 6. | Villanueva C, Colomo A, Bosch A, Concepción M, Hernandez-Gea V, Aracil C, Graupera I, Poca M, Alvarez-Urturi C, Gordillo J. Transfusion strategies for acute upper gastrointestinal bleeding. N Engl J Med. 2013;368:11-21. [Cited in This Article: ] |
| 7. | Dworzynski K, Pollit V, Kelsey A, Higgins B, Palmer K. Management of acute upper gastrointestinal bleeding: summary of NICE guidance. BMJ. 2012;344:e3412. [Cited in This Article: ] |
| 8. | Bernard B, Grangé JD, Khac EN, Amiot X, Opolon P, Poynard T. Antibiotic prophylaxis for the prevention of bacterial infections in cirrhotic patients with gastrointestinal bleeding: a meta-analysis. Hepatology. 1999;29:1655-1661. [Cited in This Article: ] |
| 9. | Garcia-Tsao G, Sanyal AJ, Grace ND, Carey WD. Prevention and management of gastroesophageal varices and variceal hemorrhage in cirrhosis. Am J Gastroenterol. 2007;102:2086-2102. [Cited in This Article: ] |
| 10. | D’Amico G, Pietrosi G, Tarantino I, Pagliaro L. Emergency sclerotherapy versus vasoactive drugs for variceal bleeding in cirrhosis: a Cochrane meta-analysis. Gastroenterology. 2003;124:1277-1291. [Cited in This Article: ] |
| 11. | Al-Osaimi AM, Caldwell SH. Medical and endoscopic management of gastric varices. Semin Intervent Radiol. 2011;28:273-282. [Cited in This Article: ] |
| 12. | Tan PC, Hou MC, Lin HC, Liu TT, Lee FY, Chang FY, Lee SD. A randomized trial of endoscopic treatment of acute gastric variceal hemorrhage: N-butyl-2-cyanoacrylate injection versus band ligation. Hepatology. 2006;43:690-697. [Cited in This Article: ] |
| 13. | Harada T, Yoshida T, Shigemitsu T, Takeo Y, Tada M, Okita K. Therapeutic results of endoscopic variceal ligation for acute bleeding of oesophageal and gastric varices. J Gastroenterol Hepatol. 1997;12:331-335. [Cited in This Article: ] |
| 14. | Paik CN, Kim SW, Lee IS, Park JM, Cho YK, Choi MG, Chung IS. The therapeutic effect of cyanoacrylate on gastric variceal bleeding and factors related to clinical outcome. J Clin Gastroenterol. 2008;42:916-922. [Cited in This Article: ] |
| 15. | Kang EJ, Jeong SW, Jang JY, Cho JY, Lee SH, Kim HG, Kim SG, Kim YS, Cheon YK, Cho YD. Long-term result of endoscopic Histoacryl (N-butyl-2-cyanoacrylate) injection for treatment of gastric varices. World J Gastroenterol. 2011;17:1494-1500. [Cited in This Article: ] |
| 16. | Roesch W, Rexroth G. Pulmonary, cerebral and coronary emboli during bucrylate injection of bleeding fundic varices. Endoscopy. 1998;30:S89-S90. [Cited in This Article: ] |
| 17. | Rajoriya N, Forrest EH, Gray J, Stuart RC, Carter RC, McKay CJ, Gaya DR, Morris AJ, Stanley AJ. Long-term follow-up of endoscopic Histoacryl glue injection for the management of gastric variceal bleeding. QJM. 2011;104:41-47. [Cited in This Article: ] |
| 18. | Al-Ali J, Pawlowska M, Coss A, Svarta S, Byrne M, Enns R. Endoscopic management of gastric variceal bleeding with cyanoacrylate glue injection: safety and efficacy in a Canadian population. Can J Gastroenterol. 2010;24:593-596. [Cited in This Article: ] |
| 19. | Cheng LF, Wang ZQ, Li CZ, Cai FC, Huang QY, Linghu EQ, Li W, Chai GJ, Sun GH, Mao YP. Treatment of gastric varices by endoscopic sclerotherapy using butyl cyanoacrylate: 10 years’ experience of 635 cases. Chin Med J (Engl). 2007;120:2081-2085. [Cited in This Article: ] |
| 20. | Seewald S, Ang TL, Imazu H, Naga M, Omar S, Groth S, Seitz U, Zhong Y, Thonke F, Soehendra N. A standardized injection technique and regimen ensures success and safety of N-butyl-2-cyanoacrylate injection for the treatment of gastric fundal varices (with videos). Gastrointest Endosc. 2008;68:447-454. [Cited in This Article: ] |
| 21. | Kind R, Guglielmi A, Rodella L, Lombardo F, Catalano F, Ruzzenente A, Borzellino G, Girlanda R, Leopardi F, Pratticò F. Bucrylate treatment of bleeding gastric varices: 12 years’ experience. Endoscopy. 2000;32:512-519. [Cited in This Article: ] |
| 22. | Lo GH, Liang HL, Chen WC, Chen MH, Lai KH, Hsu PI, Lin CK, Chan HH, Pan HB. A prospective, randomized controlled trial of transjugular intrahepatic portosystemic shunt versus cyanoacrylate injection in the prevention of gastric variceal rebleeding. Endoscopy. 2007;39:679-685. [Cited in This Article: ] |
| 23. | Procaccini NJ, Al-Osaimi AM, Northup P, Argo C, Caldwell SH. Endoscopic cyanoacrylate versus transjugular intrahepatic portosystemic shunt for gastric variceal bleeding: a single-center U.S. analysis. Gastrointest Endosc. 2009;70:881-887. [Cited in This Article: ] |
| 24. | Mahadeva S, Bellamy MC, Kessel D, Davies MH, Millson CE. Cost-effectiveness of N-butyl-2-cyanoacrylate (histoacryl) glue injections versus transjugular intrahepatic portosystemic shunt in the management of acute gastric variceal bleeding. Am J Gastroenterol. 2003;98:2688-2693. [Cited in This Article: ] |
| 25. | Tripathi D, Hayes PC. Endoscopic therapy for bleeding gastric varices: to clot or glue? Gastrointest Endosc. 2008;68:883-886. [Cited in This Article: ] |
| 26. | Williams SG, Peters RA, Westaby D. Thrombin--an effective treatment for gastric variceal haemorrhage. Gut. 1994;35:1287-1289. [Cited in This Article: ] |
| 27. | Ramesh J, Limdi JK, Sharma V, Makin AJ. The use of thrombin injections in the management of bleeding gastric varices: a single-center experience. Gastrointest Endosc. 2008;68:877-882. [Cited in This Article: ] |
| 28. | McAvoy NC, Plevris JN, Hayes PC. Human thrombin for the treatment of gastric and ectopic varices. World J Gastroenterol. 2012;18:5912-5917. [Cited in This Article: ] |
| 29. | Przemioslo RT, McNair A, Williams R. Thrombin is effective in arresting bleeding from gastric variceal hemorrhage. Dig Dis Sci. 1999;44:778-781. [Cited in This Article: ] |
| 30. | Barrio J, Ripoll C, Bañares R, Echenagusia A, Catalina MV, Camúñez F, Simó G, Santos L. Comparison of transjugular intrahepatic portosystemic shunt dysfunction in PTFE-covered stent-grafts versus bare stents. Eur J Radiol. 2005;55:120-124. [Cited in This Article: ] |
| 31. | Tripathi D. Therapies for bleeding gastric varices: is the fog starting to clear? Gastrointest Endosc. 2009;70:888-891. [Cited in This Article: ] |
| 32. | Hong CH, Kim HJ, Park JH, Park DI, Cho YK, Sohn CI, Jeon WK, Kim BI, Hong HP, Shin JH. Treatment of patients with gastric variceal hemorrhage: endoscopic N-butyl-2-cyanoacrylate injection versus balloon-occluded retrograde transvenous obliteration. J Gastroenterol Hepatol. 2009;24:372-378. [Cited in This Article: ] |
| 33. | Choi YH, Yoon CJ, Park JH, Chung JW, Kwon JW, Choi GM. Balloon-occluded retrograde transvenous obliteration for gastric variceal bleeding: its feasibility compared with transjugular intrahepatic portosystemic shunt. Korean J Radiol. 2003;4:109-116. [Cited in This Article: ] |
| 34. | Saad WE, Darcy MD. Transjugular Intrahepatic Portosystemic Shunt (TIPS) versus Balloon-occluded Retrograde Transvenous Obliteration (BRTO) for the Management of Gastric Varices. Semin Intervent Radiol. 2011;28:339-349. [Cited in This Article: ] |
| 35. | Mishra SR, Chander Sharma B, Kumar A, Sarin SK. Endoscopic cyanoacrylate injection versus beta-blocker for secondary prophylaxis of gastric variceal bleed: a randomised controlled trial. Gut. 2010;59:729-735. [Cited in This Article: ] |
| 36. | Hung HH, Chang CJ, Hou MC, Liao WC, Chan CC, Huang HC, Lin HC, Lee FY, Lee SD. Efficacy of non-selective β-blockers as adjunct to endoscopic prophylactic treatment for gastric variceal bleeding: a randomized controlled trial. J Hepatol. 2012;56:1025-1032. [Cited in This Article: ] |
| 37. | Tripathi D, Therapondos G, Jackson E, Redhead DN, Hayes PC. The role of the transjugular intrahepatic portosystemic stent shunt (TIPSS) in the management of bleeding gastric varices: clinical and haemodynamic correlations. Gut. 2002;51:270-274. [Cited in This Article: ] |
| 38. | Jang SY, Kim GH, Park SY, Cho CM, Tak WY, Kim JH, Choe WH, Kwon SY, Lee JM, Kim SG. Clinical outcomes of balloon-occluded retrograde transvenous obliteration for the treatment of gastric variceal hemorrhage in Korean patients with liver cirrhosis: a retrospective multicenter study. Clin Mol Hepatol. 2012;18:368-374. [Cited in This Article: ] |
| 39. | Cho SK, Shin SW, Yoo EY, Do YS, Park KB, Choo SW, Han H, Choo IW. The short-term effects of balloon-occluded retrograde transvenous obliteration, for treating gastric variceal bleeding, on portal hypertensive changes: a CT evaluation. Korean J Radiol. 2007;8:520-530. [Cited in This Article: ] |
| 40. | Tanihata H, Minamiguchi H, Sato M, Kawai N, Sonomura T, Takasaka I, Nakai M, Sahara S, Nakata K, Shirai S. Changes in portal systemic pressure gradient after balloon-occluded retrograde transvenous obliteration of gastric varices and aggravation of esophageal varices. Cardiovasc Intervent Radiol. 2009;32:1209-1216. [Cited in This Article: ] |
| 41. | Lee YT, Chan FK, Ng EK, Leung VK, Law KB, Yung MY, Chung SC, Sung JJ. EUS-guided injection of cyanoacrylate for bleeding gastric varices. Gastrointest Endosc. 2000;52:168-174. [Cited in This Article: ] |
| 42. | Binmoeller KF, Weilert F, Shah JN, Kim J. EUS-guided transesophageal treatment of gastric fundal varices with combined coiling and cyanoacrylate glue injection (with videos). Gastrointest Endosc. 2011;74:1019-1025. [Cited in This Article: ] |
| 43. | Orozco H, Mercado MA. The evolution of portal hypertension surgery: lessons from 1000 operations and 50 Years’ experience. Arch Surg. 2000;135:1389-193; discussion 1394. [Cited in This Article: ] |
| 44. | Galloway JR, Henderson JM. Management of variceal bleeding in patients with extrahepatic portal vein thrombosis. Am J Surg. 1990;160:122-127. [Cited in This Article: ] |
| 45. | Orloff MJ, Orloff MS, Girard B, Orloff SL. Bleeding esophagogastric varices from extrahepatic portal hypertension: 40 years’ experience with portal-systemic shunt. J Am Coll Surg. 2002;194:717-28; discussion 728-30. [Cited in This Article: ] |
| 46. | Mishra SR, Sharma BC, Kumar A, Sarin SK. Primary prophylaxis of gastric variceal bleeding comparing cyanoacrylate injection and beta-blockers: a randomized controlled trial. J Hepatol. 2011;54:1161-1167. [Cited in This Article: ] |
| 47. | Katoh K, Sone M, Hirose A, Inoue Y, Fujino Y, Onodera M. Balloon-occluded retrograde transvenous obliteration for gastric varices: the relationship between the clinical outcome and gastrorenal shunt occlusion. BMC Med Imaging. 2010;10:2. [Cited in This Article: ] |