- 1Department of Community Nursing, Preventive Medicine and Public Health and History of Science, Faculty of Health Sciences, University of Alicante, Alicante, Spain
- 2Pandemic Centre, Department of Global Public Health and Primary Care, Faculty of Medicine, University of Bergen, Bergen, Norway
- 3CIBER for Epidemiology and Public Health, Health Institute Carlos III, Madrid, Spain
- 4Unit for Migration and Health, Norwegian Public Health Institute, Oslo, Norway
Background: The coronavirus (COVID-19) pandemic and control measures adopted have had a disproportionate impact on workers, with migrants being a group specifically affected but poorly studied. This scoping review aims to describe the evidence published on the impact of the COVID-19 pandemic on the physical and mental health of migrant workers.
Methods: Papers written in English covering physical and mental health among international migrant workers during the COVID-19 pandemic, retrieved from six electronic databases searched on July 31, 2021, were included. A total of 1,096 references were extracted, of which 26 studies were finally included.
Results: Most of the migrant populations studied were born in Asia (16 of 26) and Latin America (8 of 26) and were essential workers (15 of 26). Few studies described the length of stay in the host country (9 of 26), the legal status of the migrant population (6 of 26), or established comparison groups (7 of 26). Ten studies described COVID-19 outbreaks with high infection rates. Fourteen studies evaluated mental health (anxiety, depression, worries, fears, stress, and post-traumatic stress disorder). Three of the 26 studies presented collateral positive effects of the COVID-19 pandemic because of improved hygiene.
Conclusion: There is a limited number of original publications related to the impact of the COVID-19 pandemic on the physical and mental health of migrant workers around the world. These publications mainly focus on migrants born in Asia and Latin America. The physical, long-term impact of the COVID-19 pandemic has, so far, not been evaluated. The positive collateral effects of improving healthcare conditions for migrant workers should also be further investigated.
Introduction
The COVID-19 pandemic and the measures adopted to prevent and control its spread have had an enormous impact on the global labor force, changing working and employment conditions, developing new ways of working from home and transforming safe working places into potential infection zones. The impact on the working population has been uneven and has widened social gaps (1). It is known that type of work, working conditions, and social security coverage are among the determinants of health (2, 3). As an airborne infection, the SARS-CoV-2 virus enhances the relevance of epidemiological factors in evaluating the impact of disease among workers. In this context, epidemiological factors include occupational exposure to risk of infection, the existence and quality of occupational health services, the efficacy of diagnosing, tracing and following-up of cases and contacts at work, and the possibility of having to comply with isolation and quarantine measures (4–6).
Migration is an independent determinant of health (7). Migrants have been especially hit by the COVID-19 pandemic in terms of disease and economic consequences, and the role of the different factors underlying this over-representation is not yet clear (8, 9). One possible reason is related to migrants as labor force (10). Migrants are over-represented among essential workers in low-skill professions (cleaners, helpers, construction, and industry) and have generally poorer working conditions, are more often temporally and illegally engaged, and suffer higher unemployment rates (11, 12). In Europe, migrant workers constitute 17% of the labor force (13). The pandemic has further worsened migrants' labor situation, with a relatively bigger increase in unemployment rates compared to non-migrants, and by being less often subject to compensation subsidies and social security help (14). As essential workers, migrants who retained their employment during the pandemic have been under-represented in teleworking and are at increased danger of exposure to COVID-19. Migrants, in general, have been less tested than the majority population. Undocumented migrants are especially afraid of being tested and of the consequences of positive test results (15). Additionally, some labor migrant groups rely on their employers' organization of the workplace according to COVID-19 protocol to be able to comply with isolation and quarantine measures (9).
After the first wave of the pandemic from March to July 2020, which was mostly linked to international travel (16), COVID-19 outbreaks were detected in various occupational settings, often within health care, agriculture, services, and construction, where migrants are over-represented (12). This has not only increased the risk of infection for migrants and their families, in some cases these outbreaks have contributed to the stigma and discrimination migrants face, which might have further increased their risk of disease (17). In some places, access to the healthcare system, specifically to occupational health services, is restricted for non-nationals or temporary workers, further increasing the risk of infection (8).
In this scenario, the health of labor migrants has probably deteriorated more than that of other workers during the pandemic because of higher exposure, higher susceptibility, and worse consequences of the disease (18). Although scientific research on COVID-19 pandemic is being published at an astonishingly fast pace, it has been suggested that the health of labor migrants has been neglected (19). To shed light on this particularly vulnerable group of migrants in this review, we describe the evidence published on the impact of the COVID-19 pandemic on the physical and mental health of labor migrants.
Materials and Methods
Study Design
This scoping review aims to describe published evidence on the impact of the COVID-19 pandemic on the health (physical and mental) of migrant workers. In our study, we used the methodological approach proposed by Arksey and O'Malley to enable the replication and strengthen methodological rigor (20).
The inclusion criteria for the scoping review were:
1) The studies must be written in English.
2) The studies must cover three topics: health (physical and mental), international migrant workers, and COVID-19.
The exclusion criteria for the scoping review were:
1) Commentaries, protocols, brief reports, perspectives, research letters, letters to the editor, conference abstracts, systematic comparative assessment, narrative and systematic reviews.
2) Studies describing possible risks or stress factors for COVID-19 but not analyzing their impact on health.
Search Strategy
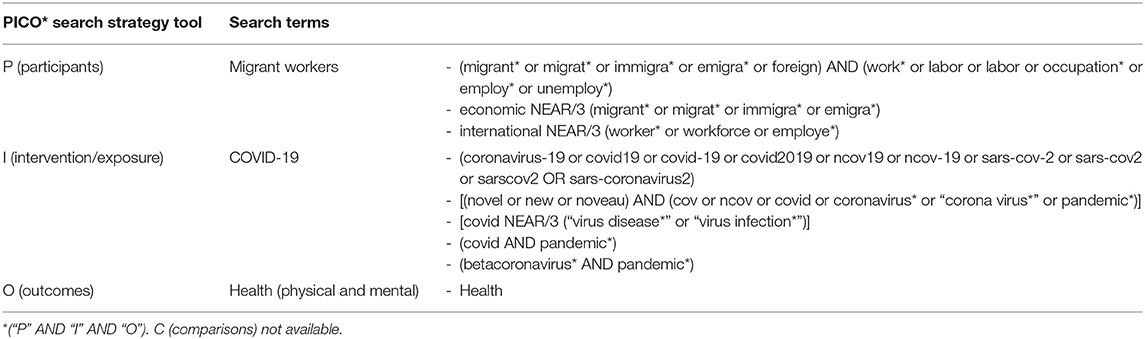
We selected six electronic databases covering a wide range of disciplines and methodologies: Scopus, Web of Science, CINAHL, Medline, PsycINFO, and Embase. The terms and strings were designed with the help of specialist librarians from the Universities of Bergen and Alicante during July 2021. To define our search terms, we used the PICO search strategy tool (Table 1). Only temporal limits were established on the searches (2019–2021) due to the discovery and global spread of a new coronavirus variant (SARS-Cov-2) in December 2019 in Wuhan (China). Because of the nature of the databases, our search strategies combined Medical Subject Heading (MeSH) and free-text terms. Search terms were truncated to guarantee all relevant articles were included in the analysis. The last review and extraction of information from the corresponding databases was performed on July 31 2021. The results of the electronic search were exported to the Endnote and Mendeley bibliographic managers and duplicates were eliminated.
Data Extraction
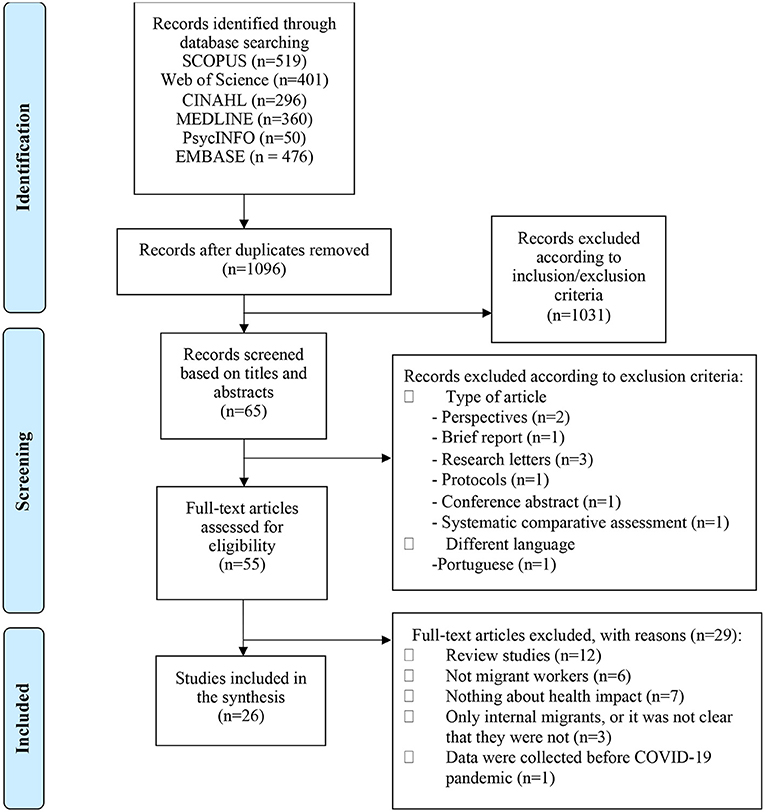
After the bibliographic search in the selected databases, a total of 2,102 results were obtained (519 in Scopus, 401 in Web of Science, 296 in CINAHL, 360 in Medline, 50 in PsycINFO, and 476 in Embase). After removing duplicates, we ended up with 1,096 papers. Potentially relevant articles were screened by title and abstract by two of the authors (AO, PB), excluding those that did not follow the inclusion criteria. If the abstracts were not informative enough, the articles were selected for further analysis in the next round of review. Differences of opinion with regard to eligibility in the first round were resolved through consensus adjudication between the four authors. A total of 55 papers were selected in the first round. Systematic reviews and narrative reviews were included to assess their bibliographies and we ensured that all the studies listed in those reviews were captured in our database searches.
For selected papers, the full text was independently reviewed by the two authors (AO, PB) and all doubts were discussed by the whole research team. Data was extracted from the documents using an Excel template previously designed to collect and summarize this data. The information registered in the template included: main characteristics of the articles (author name, year of publication, the country where the research was carried out, and journal name), design and data collection technique (e.g., type of article, type of research, and source of primary/secondary data), properties of the sample studied (e.g., sample size, sex, age, country, length of stay, legal status, occupation, and a comparison group if any), objectives, main outcomes, main results, limitations, and conclusions. At the beginning of the full-text review, we carried out a pilot using selected sample articles to test and refine the template and discuss discrepancies with all four researchers. The main question to agree upon was the inclusion of papers focusing on social determinants of health. We agreed to include papers that studied the associations between the COVID-19 pandemic and these determinants and their impact on the health of migrant workers. To guide and structure our results according to the main objective of our scoping review, we classified the included articles by type of outcome: positive (if health status improved or remained the same) or negative (if health status worsened). Negative outcomes include mental (e.g., anxiety, stress, or depression) or physical (e.g., headache or chest pain) conditions that emerged or worsened due to the pandemic and the preventive and control measures adopted. In this regard, reported COVID-19 cases were categorized into physical outcomes. One article reported both types of outcomes and we therefore included it in both groups. In order to facilitate the classification of occupational sectors for the migrant population, the official industry guidelines by the United States Department of Homeland Security (21) and WHO classification (22) were used to identify essential workers and the healthcare workforce, respectively.
A total of 26 papers met the inclusion criteria for this scoping review. Figure 1 shows the screening and selection process followed (23).
Results
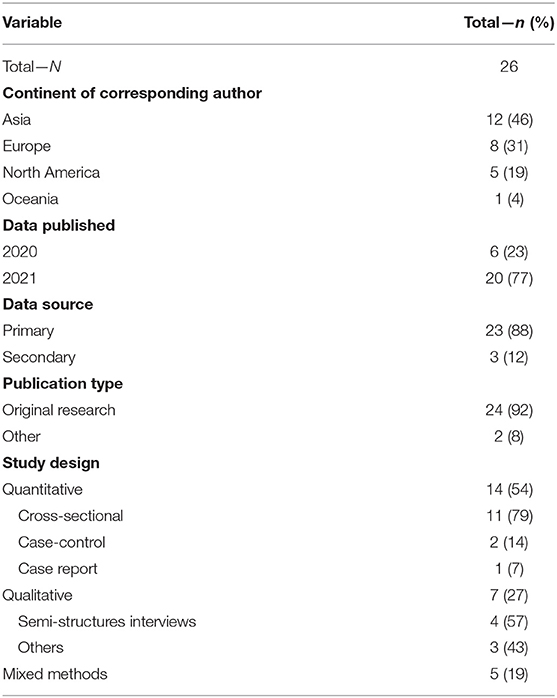
Of the 26 included studies (24–49) almost half (12 of 26) were conducted in Asia (24, 26, 30, 32–35, 37, 41, 44, 47, 49) and 8 in Europe. Fourteen papers used a quantitative design (24, 27, 28, 30, 32, 33, 35, 36, 40, 42–44, 46, 48), 5 applied mixed methods (29, 31, 34, 38, 45) and 23 used primary data sources (24–29, 31, 32, 34, 36–49) (Table 2).
Figure 2 shows the geographical, legal, and occupational characteristics of the migrant workers in the 26 studies. Most immigrant populations represented in the studies originated from countries in Asia (16 of 26 studies) (24, 26, 27, 31–34, 37, 38, 41–44, 47–49) and Latin America (8 of 26) (25, 28, 29, 38, 39, 42, 44, 46). Other characteristics of the studied populations were often not described in the methodology of the papers: only 9 studies clearly described migrants' length of stay in the host country (24, 27, 31, 32, 37, 39, 41, 43, 48), most of which were long stays (five or more years) and migrants' legal status was not specified in 20 studies (26–30, 32–34, 36, 37, 39, 40, 42–49). Seven studies had a comparison group (29, 30, 33, 35, 36, 40, 45), most frequently the majority population (6 of 7 studies) (30, 33, 35, 36, 40, 45). Regarding occupation sectors, most of the migrant population were considered essential workers in sectors related to healthcare (6 of 26) (24, 27, 31, 33, 36, 39) and other essential sectors (11 of 26) (25–30, 35, 38, 43, 45, 46) such as agriculture or construction.
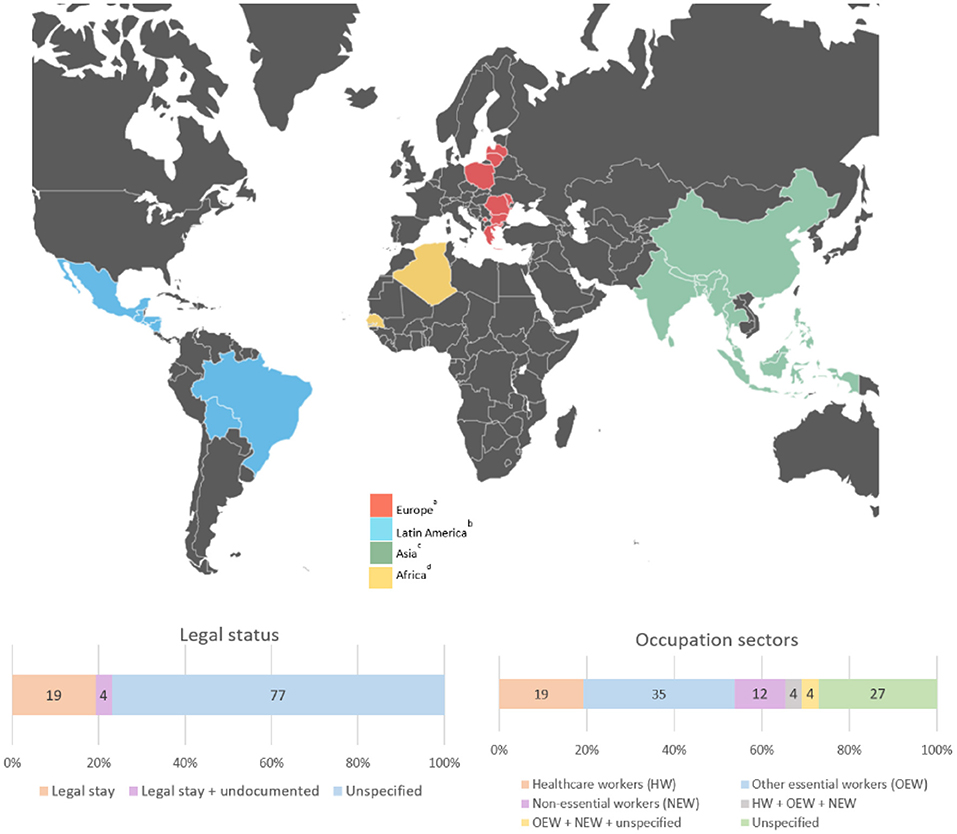
Figure 2. Country of origin, legal status, and occupation sectors of the migrant samples of the 26 studies selected. aRomania, Poland, Greece, Latvia, Moldova, Lithuania, Bulgaria, and Kosovo. bMexico, El Salvador, Guatemala, Honduras, Nicaragua, Bolivia, and Brazil. cPhilipines, India, Sri Lanka, Nepal, Bhutan, Myanmar, Bangladesh, Malaysia, Thailand, China, and Indonesia. dAlgeria and Senegal.
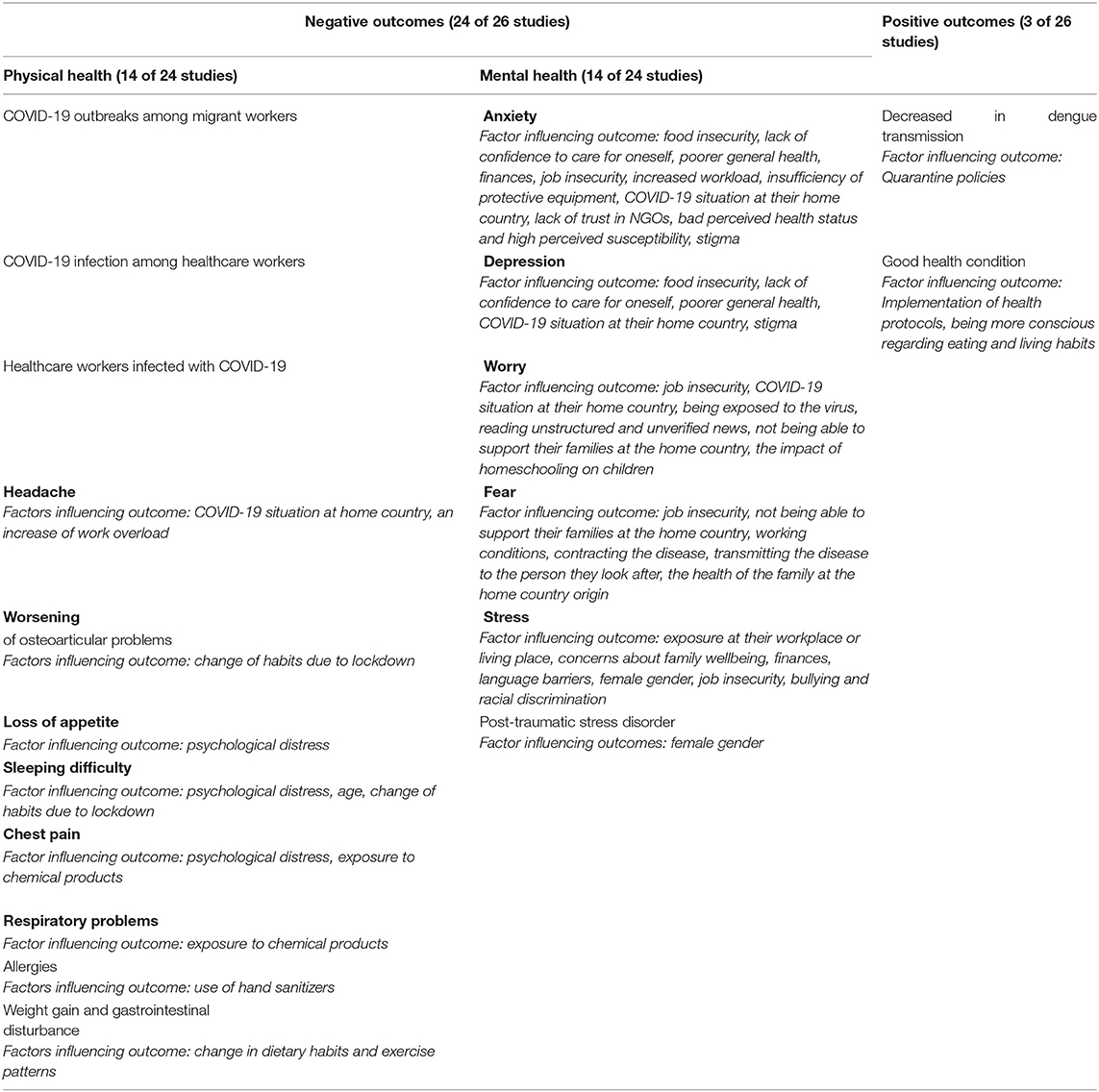
As showed in Table 3, most of the selected studies found negative outcomes of the COVID-19 pandemic on the health of migrant workers (24 of 26) (24–29, 31–33, 35–49). Fourteen studies described the impact of COVID-19 on migrants' physical health (25, 27, 28, 33, 35, 36, 39–42, 44–46, 49), 10 studies described COVID-19 outbreaks (25, 27, 28, 33, 35, 36, 40, 42, 45, 46), and the remaining 4 studies mentioned other physical problems such as headaches, sleeping difficulty, respiratory problems, and chest pain (39, 41, 44, 49). Fourteen studies assessed the effects of COVID-19 on mental health outcomes, including anxiety, depression, worry, fear, stress, and post-traumatic stress disorder (24, 26, 29, 31, 32, 37–39, 41, 43, 44, 47–49). Most of these studies linked psychological distress with migrants' economic/financial situation, loss of jobs, food insecurity, exposure to the virus, and/or situation of family members. Anxiety, depression, and stress were related to discrimination and stigma (31, 41, 43, 48, 49).
Three of the 26 studies presented collateral positive effects of the COVID-19 pandemic. One mentioned a decrease in dengue transmission among migrant workers in dormitory sites in Singapore (30), the second mentioned good health conditions for Indonesian migrant workers because of national health protocols being implemented (34), and the third discussed the adoption of new healthy behaviors and the self-perception of being healthier than before the pandemic (41).
Discussion
This scoping review provides an overview of the published evidence of the impact of the COVID-19 pandemic on the health of migrant workers. It spans the duration of the pandemic until July 2021. We found a small number of original articles focusing on the negative impact of the pandemic on the health of migrant workers, mainly related to COVID-19 outbreaks and the consequences on mental health.
Most of the migrant populations studied during the pandemic worked in occupations defined as essential. Migrant workers are central to the proper functioning of high-income countries and the recent COVID-19 outbreak has only emphasized this fact. Measures to contain the spread of the virus have involved lockdowns and mobility restrictions, while migrant essential workers have had to work in precarious working conditions with a high risk of infection due to limited health and safety protection measures (9). All of this appears to have been detrimental to migrants' mental health, both for those who have remained in destination countries (50) and for those who have been forced to return to their countries of origin (51). According to our results and the research on migrant health in general (52, 53), mental health of migrant workers during COVID-19 seems to be of great interest to researchers. Our research provides evidence on the challenges migrant workers face (e.g., fear of infection, job insecurity, family responsibilities, material and medical needs, and discrimination) and can guide the actions needed to reduce their impact (40, 41, 54).
Of the studies selected in this review, more than half focused on the physical health of migrant workers, but most reported short-term infectious outbreaks. A few articles reported other physical health problems. Among these, respiratory problems, chest pain, and allergies were associated with exposure to chemical products such as hand sanitizer and cleaning products. A limited number of articles also identified sleeping difficulties associated with psychological distress and change in habits due to the lockdown. One study mentioned weight gain and gastrointestinal disturbance because of changes in dietary habits and exercise patterns. Some evidence has been published on isolation, quarantine, and confinement and their effect on physical activity reduction and dietary changes as possible risk factors for the development of chronic diseases in the general population (55–57). All these issues affecting the migrant population require in-depth research.
Most of the studies identified in this scoping review focused on the first wave of the pandemic and therefore do not provide information on the long-term consequences. As is otherwise common in the literature related to the pandemic, research related to COVID-19 and the health of migrant populations has focused on the negative effects of the pandemic and its control and preventive measures. However, for many essential workers, sanitary conditions have improved during the pandemic because of stricter hygiene norms. We found a few studies on the positive impact of COVID-19 pandemic on the health of migrants. Authors like Cornet et al. mentioned the importance of following up on these positive results in the migrant population to sustain the positive changes after the pandemic (58). In addition, Huso et al. suggested the importance of implementing specific government healthcare protocols and quarantine measures that guarantee access to essential services to maintain good health (59).
Most of the studies included in the review had methodological limitations and provided little descriptive information on the migrant samples. Better data related to length of stay, legal status or establishing comparison groups, for example, would have contextualized the results of the studies. Finally, very few studies cover African migrant workers during the pandemic, despite the fact that this migrant group has grown considerably in the last 15 years (60). Although concerns have been raised on the matter, research remains scarce (61).
Table 4 provides a recommendation list for future study based on the research gaps identified in this article.
Our scoping review has some limitations. Due to the emergence and impact of COVID-19, numerous studies have been published within a short period of time. As a result, we have found high heterogeneity among the studies in terms of design and methodology, which has made it difficult for us to synthesize and compare results. The authors had to make difficult decisions on the inclusion criteria to maintain rigor and achieve an adequate number of selected articles. We decided to exclude gray literature and research published in languages other than English. It is therefore possible that we missed some relevant research work on the subject. However, numerous multidisciplinary databases were consulted to collect as many studies as possible.
Conclusions
The COVID-19 pandemic has caused widespread economic and social disruption, affecting the lives, livelihoods, and health of people across the globe. The pandemic has also exacerbated existing inequalities among vulnerable groups such as migrant workers. There has been an exponential increase in studies related to the pandemic in general, but the findings of this scoping review indicate that there is a limited number of original publications related to the impact of the COVID-19 pandemic on the health of labor migrants. In particular, the physical long-term impact of the COVID-19 pandemic and the positive collateral effects of improving healthcare conditions for migrant workers should be further investigated. We hope our findings will help focus research attention to important areas that have been overlooked, as well as highlight the need for governments and health institutions to put in place measures to ensure that the health and rights of migrant workers are protected.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Author Contributions
AO-A, PB, ER, and ED were involved in all stages of the project and contributed to reviewing the data and writing the manuscript. ER and ED conceptualized the review and provided background information. AO-A and PB designed the search strategy and conducted the screening, data extraction, and synthesis of the literature information. All authors have approved the final manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2022.816597/full#supplementary-material
References
1. Shadmi E, Chen Y, Dourado I, Faran-Perach I, Furler J, Hangoma P, et al. Health equity and COVID-19: global perspectives. Int J Equity Health. (2020) 19:1–16. doi: 10.1186/s12939-020-01218-z
2. Montero-Moraga JM, Benavides FG, Lopez-Ruiz M. Association between informal employment and health status and the role of the working conditions in Spain. Int J Heal Serv. (2020) 50:199–208. doi: 10.1177/0020731419898330
3. Puig-Barrachina V, Giró P, Artazcoz L, Bartoll X, Cortés-Franch I, Fernández A, et al. The impact of active labour market policies on health outcomes: a scoping review. Eur J Public Health. (2020) 30:36–42. doi: 10.1093/eurpub/ckz026
4. Burdorf A, Porru F, Rugulies R. The COVID-19 (Coronavirus) pandemic: consequences for occupational health. Scand J Work Environ Heal. (2020) 46:229–30. doi: 10.5271/sjweh.3893
5. Benavides FG. Workers' health and COVID-19. Arch Prev Riesgos Labor. (2020) 23:154–8. doi: 10.12961/aprl.2020.23.02.02
6. Sargeant M, Tucker E. Layers of vulnerability in occupational safety and health for migrant workers: case studies from canada and the UK. Policy Pract Heal Saf. (2009) 7:51–73. doi: 10.1080/14774003.2009.11667734
8. Fassani F, Mazza J. A Vulnerable Workforce: Migrant Workers in the COVID-19 Pandemic. Luxembourg: Publications Office of the European Union (2020).
9. Reid A, Rhonda-Perez E, Schenker MB. Migrant workers, essential work, and COVID-19. Am J Ind Med. (2021) 64:73–7. doi: 10.1002/ajim.23209
10. The Lancet. The plight of essential workers during the COVID-19 pandemic. Lancet. (2020) 395:1587. doi: 10.1016/S0140-6736(20)31200-9
11. Arici C, Ronda-Pérez E, Tamhid T, Absekava K, Porru S. Occupational health and safety of immigrant workers in italy and spain: a scoping review. Int J Environ Res Public Health. (2019) 16:1–32. doi: 10.3390/ijerph16224416
12. Fasani F, Mazza J. Immigrant key workers: their contribution to Europe's COVID-19 Response. IZA Discussion Paper (2020) 13178. doi: 10.2139/ssrn.3584941
13. Fair Employment Conditions for Migrant Workers in the EU—How to Provide Better Support Services for Migrants? International Labour Organization. (2020). Available online at: http://www.ilo.org/budapest/whats-new/WCMS_757579/lang–en/index.htm (accessed November 15, 2021).
14. “Left with Nothing”: Australia's Migrant Workforce Face Destitution Without Coronavirus Safety Net. Australian immigration and asylum. The Guardian. (2020). Available online at: https://www.theguardian.com/australia-news/2020/apr/01/left-with-nothing-australias-migrant-workforce-face-destitution-without-coronavirus-safety-net?CMP=Share_iOSApp_Other (accessed November 15, 2021).
15. Cervantes L, Martin M, Frank MG, Farfan JF, Kearns M, Rubio LA, et al. Experiences of latinx individuals hospitalized for COVID-19: a qualitative study. JAMA Netw Open. (2021) 4:1–15. doi: 10.1001/jamanetworkopen.2021.0684
16. Ribeiro SP, Dáttilo W, Barbosa DS, Coura-Vital W, Das Chagas IAS, Dias CP, et al. Worldwide covid-19 spreading explained: traveling numbers as a primary driver for the pandemic. An Acad Bras Cienc. (2020) 92:1–10. doi: 10.1590/0001-3765202020201139
17. Ransing R, Ramalho R, Filippis R De, Isioma M, Karaliuniene R, Orsolini L, et al. Infectious disease outbreak related stigma and discrimination during the COVID-19 pandemic: drivers, facilitators, manifestations, and outcomes across the world. Brainm Behav Immun. (2020) 89:555–8. doi: 10.1016/j.bbi.2020.07.033
18. Orcutt M, Patel P, Burns R, Hiam L, Aldridge R, Devakumar D, et al. Global call to action for inclusion of migrants and refugees in the COVID-19 response. Lancet. (2020) 395:1482–3. doi: 10.1016/S0140-6736(20)30971-5
19. Liem A, Wang C, Wariyanti Y, Latkin CA, Hall BJ. The neglected health of international migrant workers in the COVID-19 epidemic. Lancet Psychiatry. (2020) 7:e20. doi: 10.1016/S2215-0366(20)30076-6
20. Arksey H, O'Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol Theory Pract. (2005) 8:19–32. doi: 10.1080/1364557032000119616
21. Wales B. Guidance on the Essential Critical Infrastructure Workforce: Ensuring Community National Resilience in COVID-19 Response. Cybersecurity Infrastruct Secur Agency (CISA) (2020). Available online at: https://www.cisa.gov/publication/guidance-essential-critical-infrastructure-workforce (accessed November 15, 2021)
22. World Health Organization. Classifying Health Workers: Mapping Occupations to the International Standard Classification. Geneva: World Health Organization (2008). p. 1–14.
23. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. PLoS Med. (2021) 18:1–15. doi: 10.1371/journal.pmed.1003583
24. Attal JH, Lurie I, Neumark Y. A rapid assessment of migrant careworkers' psychosocial status during Israel's COVID-19 lockdown. Isr J Health Policy Res. (2020) 9:61. doi: 10.1186/s13584-020-00422-0
25. Lauzardo M, Kovacevich N, Dennis A, Myers P, Flocks J, Morris JG. An outbreak of COVID-19 among H-2A temporary agricultural workers. Am J Public Health. (2021) 111:571–3. doi: 10.2105/AJPH.2020.306082
26. Jamil R, Dutta U. Centering the margins: the precarity of Bangladeshi low-income migrant workers during the time of COVID-19. Am Behav Sci. (2021) 65:1384–405. doi: 10.1177/00027642211000397
27. Zhang M, Gurung A, Anglewicz P, Yun K. COVID-19 and immigrant essential workers: Bhutanese and burmese refugees in the United States. Public Health Rep. (2021) 136:117–23. doi: 10.1177/0033354920971720
28. Mema S, Frosst G, Hanson K, Yates C, Anderson A, Jacobsen J, et al. COVID-19 outbreak among temporary foreign workers in British Columbia, March to May (2020). Canada Commun Dis Rep. (2021) 47:5–10. doi: 10.14745/ccdr.v47i01a02
29. Quandt SA, LaMonto NJ, Mora DC, Talton JW, Laurienti PJ, Arcury TA. COVID-19 pandemic among immigrant latinx farmworker and non-farmworker families: a rural–urban comparison of economic, educational, healthcare, and immigration concerns. New Solut A J Environ Occup Heal Policy. (2021) 30:30–47. doi: 10.1177/1048291121992468
30. Lim JT, Dickens BL, Ong J, Aik J, Lee VJ, Cook AR, et al. Decreased dengue transmission in migrant worker populations in Singapore attributable to SARS-CoV-2 quarantine measures. J Travel Med. (2021) 28:1–5. doi: 10.1093/jtm/taaa228
31. Song J, McDonald C. Experiences of New Zealand registered nurses of Chinese ethnicity during the COVID-19 pandemic. J Clin Nurs (John Wiley Sons, Inc). (2021) 30:757–64. doi: 10.1111/jocn.15607
32. Yeung NCY, Huang B, Lau CYK, Lau JTF. Feeling anxious amid the covid-19 pandemic: Psychosocial correlates of anxiety symptoms among filipina domestic helpers in hong kong. Int J Environ Res Public Health. (2020) 17:1–15. doi: 10.3390/ijerph17218102
33. Wong LY, Tan AL, Leo Y-S, Lee VJM, Toh MPHS. Healthcare workers in Singapore infected with COVID-19:23 January-17 April (2020). Influenza Other Respi Viruses. (2021) 15:218–26. doi: 10.1111/irv.12803
34. Kusumastuti A, Arawindha U, Harjo IWW. Indonesia Migrant Worker's Strategy Toward Covid-19: Study of Migrant's Knowledge and Host Countries' Policy. In Department of Sociology, Universitas Brawijaya, Malang: IEOM Society. (2020).
35. Koh D. Migrant workers and COVID-19. Occup Environ Med. (2020) 77:634–6. doi: 10.1136/oemed-2020-106626
36. Lombardi A, Mangioni D, Consonni D, Cariani L, Bono P, Cantu AP, et al. Seroprevalence of anti-SARS-CoV-2 IgG among healthcare workers of a large university hospital in Milan, Lombardy, Italy: a cross-sectional study. BMJ Open. (2021) 11:e047216. doi: 10.1136/bmjopen-2020-047216
37. Yee K, Peh HP, Tan YP, Teo I, Tan EUT, Paul J, et al. Stressors and coping strategies of migrant workers diagnosed with COVID-19 in Singapore: a qualitative study. BMJ Open. (2021) 11:e045949. doi: 10.1136/bmjopen-2020-045949
38. Burton-Jeangros C, Duvoisin A, Consoli L, Fakhoury J, Lachat S, Jackson Y. The impact of the Covid-19 pandemic and the lockdown on the health and living conditions of undocumented migrants and migrants undergoing legal status regularization. Front public Heal. (2020) 8:596887. doi: 10.3389/fpubh.2020.596887
39. de Diego-Cordero R, Tarriño-Concejero L, Lato-Molina MÁ, García-Carpintero Muñoz MÁ. COVID-19 and female immigrant caregivers in Spain: cohabiting during lockdown. Eur J Womenow Stud. (2021) 1–17. doi: 10.1177/13505068211017577
40. Hamadah H, Alahmad B, Behbehani M, Al-Youha S, Almazeedi S, Al-Haddad M, et al. COVID-19 clinical outcomes and nationality: results from a Nationwide registry in Kuwait. BMC Public Health. (2020) 20:1–9. doi: 10.1186/s12889-020-09490-y
41. Bhandari D, Kotera Y, Ozaki A, Abeysinghe S, Kosaka M, Tanimoto T. COVID-19: challenges faced by Nepalese migrants living in Japan. BMC Public Health. (2021) 21:1–14. doi: 10.1186/s12889-021-10796-8
42. Yuguero O, Calahorra M, Cuevas S, Gimenez N, Hernandez I, Lacasta JD, et al. Cross-sectional study of SARS-CoV2 clinical characteristics in an immigrant population attended in a Hospital Emergency Department in the Catalunya Health Region in Spain. J Migr Heal. (2021) 4:100055. doi: 10.1016/j.jmh.2021.100055
43. Zhang M, Gurung A, Anglewicz P, Baniya K, Mengxi Y. Discrimination and stress among Asian Refugee populations during the COVID-19 pandemic: evidence from Bhutanese and Burmese Refugees in the USA. J Racial Ethn Heal Disparities. (2021) 1–9. doi: 10.1007/s40615-021-00992-y
44. Barbato M, Thomas J. In this together: psychological wellbeing of foreign workers in the United Arab Emirates during the COVID-19 pandemic. Int J Psychol. (2021) 56:825–33. doi: 10.1002/ijop.12786
45. Boogaard LH, Sikkema RS, van Beek JHGM, Brockhoff HJ, Dalebout E, de Heus B, et al. A mixed-methods approach to elucidate SARS-CoV-2 transmission routes and clustering in outbreaks in native workers and labour migrants in the fruit and vegetable packaging industry in South Holland, the Netherlands, May to July (2020). Int J Infect Dis. (2021) 109:24–32. doi: 10.1016/j.ijid.2021.06.021
46. Corwin C, Sinnwell E, Culp K. A mobile primary care clinic mitigates an early COVID-19 outbreak among migrant farmworkers in Iowa. J Agromed. (2021) 26:346–51. doi: 10.1080/1059924X.2021.1913272
47. Kaur-Gill S, Qin-Liang Y, Hassan S. Negotiating mental health during the COVID-19 pandemic: performing migrant domestic work in contentious conditions. Am Behav Sci. (2021) 65:1406–25. doi: 10.1177/00027642211000394
48. Harjana NPA, Januraga PP, Indrayathi PA, Gesesew HA, Ward PR. Prevalence of depression, anxiety, and stress among repatriated indonesian migrant workers during the COVID-19 pandemic. Front Public Heal. (2021) 9:1–8. doi: 10.3389/fpubh.2021.630295
49. Lui ID, Vandan N, Davies SE, Harman S, Morgan R, Smith J, et al. “We also deserve help during the pandemic”: the effect of the COVID-19 pandemic on foreign domestic workers in Hong Kong. J Migr Heal. (2021) 3:100037. doi: 10.1016/j.jmh.2021.100037
50. Acharya SR, Moon DH, Chun JH, Shin YC. COVID-19 and mental health: anxiety disorders among immigrants due to COVID-19 outbreak in South Korea. Int J Psychiatry Med. (2021) 1–15. doi: 10.1177/00912174211042695
51. Habtamu K, Desie Y, Asnake M, Lera EG, Mequanint T. Psychological distress among Ethiopian migrant returnees who were in quarantine in the context of COVID-19: institution-based cross-sectional study. BMC Psychiatry. (2021) 21:1–15. doi: 10.1186/s12888-021-03429-2
52. Laue J, Diaz E, Eriksen L, Risør T. Migration health research in Norway: a scoping review. Scand J Public Health. (2021) 1–10. doi: 10.1177/14034948211032494
53. Sweileh WM, Wickramage K, Pottie K, Hui C, Roberts B, Sawalha AF, et al. Bibliometric analysis of global migration health research in peer-reviewed literature (2000-2016). BMC Public Health. (2018) 18:1–18. doi: 10.1186/s12889-018-5689-x
54. Spiritus-Beerden E, Verelst A, Devlieger I, Primdahl NL, Guedes FB, Chiarenza A, et al. Mental health of refugees and migrants during the covid-19 pandemic: the role of experienced discrimination and daily stressors. Int J Environ Res Public Health. (2021) 18:354. doi: 10.3390/ijerph18126354
55. Kirwan R, McCullough D, Butler T, Perez de Heredia F, Davies IG, Stewart C. Sarcopenia during COVID-19 lockdown restrictions: long-term health effects of short-term muscle loss. GeroScience. (2020) 42:1547–78. doi: 10.1007/s11357-020-00272-3
56. Di Stefano V, Battaglia G, Giustino V, Gagliardo A, D'Aleo M, Giannini O, et al. Significant reduction of physical activity in patients with neuromuscular disease during COVID-19 pandemic: the long-term consequences of quarantine. J Neurol. (2021) 268:20–6. doi: 10.1007/s00415-020-10064-6
57. Palmer K, Monaco A, Kivipelto M, Onder G, Maggi S, Michel JP, et al. The potential long-term impact of the COVID-19 outbreak on patients with non-communicable diseases in Europe: consequences for healthy ageing. Aging Clin Exp Res. (2020) 32:1189–94. doi: 10.1007/s40520-020-01601-4
58. Cornell S, Nickel B, Cvejic E, Bonner C, McCaffery KJ, Ayre J, et al. Positive outcomes associated with the COVID-19 pandemic in Australia. Heal Promot J Aust. (2021) 1–9. doi: 10.1002/hpja.494
59. Yi H, Ng ST, Farwin A, Pei Ting Low A, Chang CM, Lim J. Health equity considerations in COVID-19: geospatial network analysis of the COVID-19 outbreak in the migrant population in Singapore. J Travel Med. (2021) 28:taaa159. doi: 10.1093/jtm/taaa159
60. African Union Commission (AUC). Report on Labour Migration Statistics in Africa 2017. 2nd ed. Addis Ababa: AUC (2020).
61. ILO Webinar Examines Impact of COVID-19 on African Migrant Workers in the SADC and IGAD Regions. International Labour Organization. (2020). Available online at: https://www.ilo.org/africa/media-centre/articles/WCMS_764490/lang–en/index.htm (accessed November 15, 2021).
Keywords: scoping review, COVID-19, coronavirus, health, migrant workers, international workers
Citation: Oliva-Arocas A, Benavente P, Ronda E and Diaz E (2022) Health of International Migrant Workers During the COVID-19 Pandemic: A Scoping Review. Front. Public Health 10:816597. doi: 10.3389/fpubh.2022.816597
Received: 16 November 2021; Accepted: 21 January 2022;
Published: 16 February 2022.
Edited by:
Maria Rosario O. Martins, New University of Lisbon, PortugalReviewed by:
Sara Simões Dias, Polytechnic of Leiria, PortugalPrama Bhattacharya, O.P. Jindal Global University, India
Copyright © 2022 Oliva-Arocas, Benavente, Ronda and Diaz. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Adriana Oliva-Arocas, adriana.oliva@ua.es
 Adriana Oliva-Arocas
Adriana Oliva-Arocas Pierina Benavente
Pierina Benavente Elena Ronda1,3
Elena Ronda1,3