Dairy product consumption was associated with a lower likelihood of non-alcoholic fatty liver disease: A systematic review and meta-analysis
- 1Department of Clinical Epidemiology, Shengjing Hospital of China Medical University, Shenyang, China
- 2Key Laboratory of Precision Medical Research on Major Chronic Disease, Shenyang, China
- 3School of Public Health, Wannan Medical College, Wuhu, China
Background and aims: Non-alcoholic fatty liver disease (NAFLD) is one of the most common causes of chronic liver disease. Several epidemiological studies attempted to assess the association between dairy product and the likelihood of NAFLD, but the contribution of dairy consumption to NAFLD remains controversial. We conducted a meta-analysis to investigate the association between dairy product consumption and NAFLD.
Methods: We conducted a literature search using the PubMed, Web of Science and Scopus databases, we conducted a thorough search of the literature published before January 5, 2023. Combined odds ratios (ORs) and 95% confidence intervals (CIs) of NAFLD in relation to dairy product intake were estimated using random-effects models. Subgroup analysis and meta-regression were performed according to the study design, region, sex, body mass index (BMI), type of exposure, NAFLD diagnostic criteria, and exposure assessment tools.
Results: We initially identified 4,634 relevant studies, of which 25 complied with the inclusion criteria, including seven cross-sectional studies, six case–control studies and one cohort study. A total of 51,476 participants (14,546 patients with NAFLD) were included in the meta-analysis. There was an inverse association between dairy product consumption and NAFLD (OR = 0.97, 95% CI = 0.94–0.99). Subgroup analysis demonstrated that lower likelihood of NAFLD was associated with dairy product consumption in subgroups of Asian populations, women, patients diagnosed using NAFLD-related scores, patients with a BMI of 18.5–24.9 kg/m2, dairy intake assessed using a food frequency questionnaire, milk consumption, and yogurt consumption. No noteworthy connection was observed in the other subgroups.
Conclusion: Our meta-analysis findings revealed that dairy product consumption is inversely associated with NAFLD. Consumption of dairy products could help prevent the development of non-alcoholic fatty liver disease.
Introduction
In the world today, non-alcoholic fatty liver disease (NAFLD) is rapidly becoming the most prevalent form of chronic liver disease (1), affecting approximately 25 and 10% of the global adult and pediatric populations, respectively (2, 3). NAFLD is defined by steatosis of at least 5% of hepatocytes, confirmed primarily by histology or high-resolution imaging, while excluding known hepatotoxic factors such as excessive alcohol consumption, viral infections, or illicit drug use (4). International guidelines suggest that lifestyle changes linked to nutrition should be a crucial component of NAFLD therapy, although there is no agreement on the pharmacological management of NAFLD (5). Therefore, it is necessary to identify healthy dietary interventions to reduce the burden of NAFLD.
Dietary guidelines worldwide recommend milk and dairy products (6), but it remains controversial whether dairy products are associated with NAFLD. Several recent studies have shown that dairy product consumption is not associated with NAFLD (7–9). In contrast, the results of a case–control study showed that dairy product consumption was associated with a lower likelihood of NAFLD (10). However, a cross-sectional study reported an increased likelihood of NAFLD associated with dairy consumption (11). Numerous unique fatty acids found in dairy products, including short-chain fatty acids and palmitoleic acid, which resemble hormones, may have beneficial metabolic effects (12, 13). In a previous study, dairy fat was found to enhance glucose tolerance, which may increase hepatic insulin sensitivity and systemically reduce liver fat deposition (14). However, the chances of developing NAFLD were increased by dairy products (especially cheese) in another study, which could be due to saturated fatty acids in dairy products (15). These inconsistent results highlight the diverse associations between different types of dairy intake and NAFLD.
To our knowledge, although a previous meta-analysis investigated the association between dairy intake and NAFLD, the inclusion of dairy product types was neither complete nor specific (e.g., ice cream was not included) (16). Therefore, we aimed to more accurately and comprehensively estimate the impact of dairy consumption, including that of various dairy products, on NAFLD. To achieve this, we assessed the association between the consumption of dairy products, and their different types, and the development of NAFLD. Furthermore, we conducted a subgroup analysis based on the included studies’ characteristics, such as study design, dietary assessment tools, and of the study populations and regions.
Materials and methods
Database searches
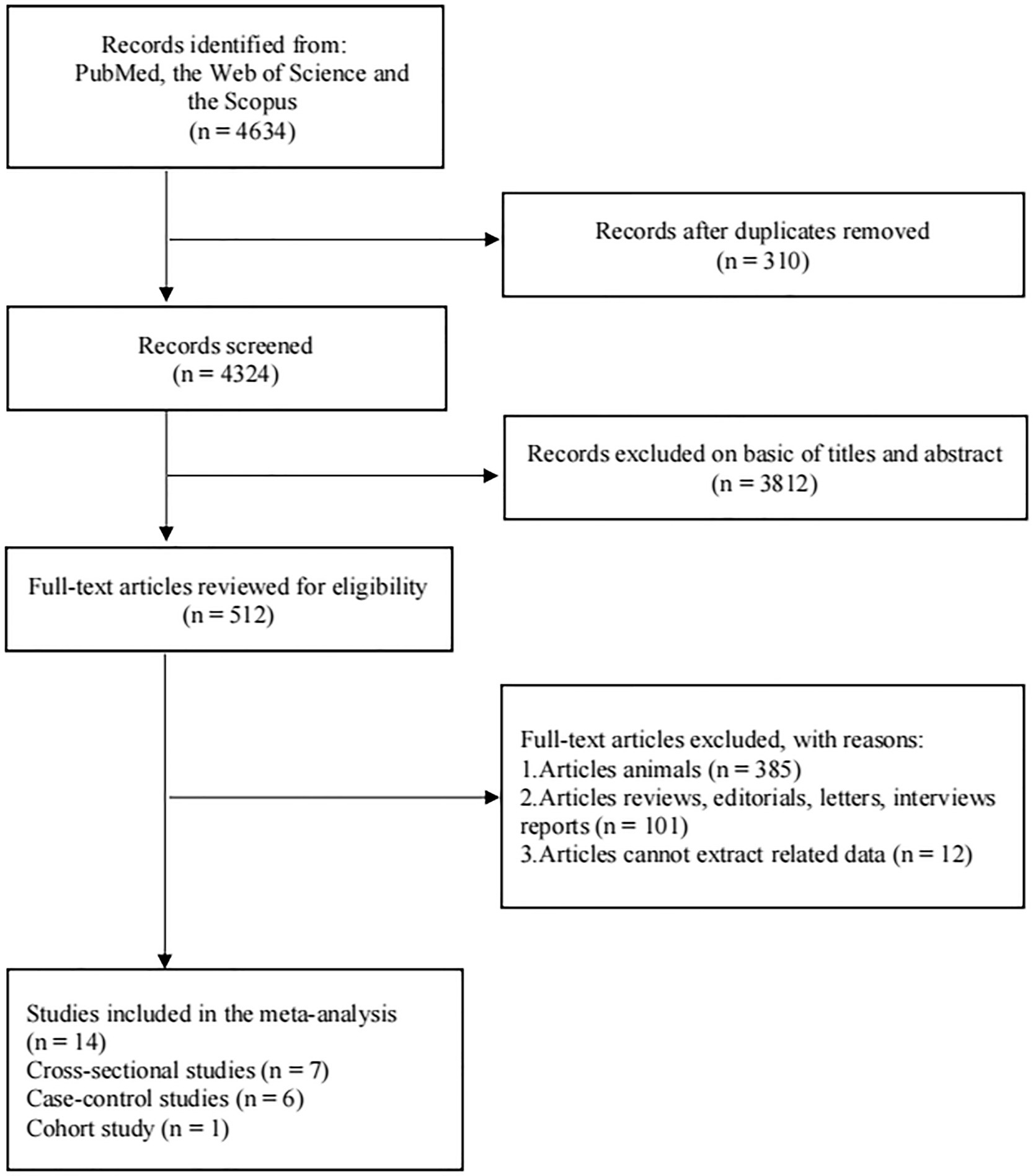
Using the PubMed, Web of Science and Scopus databases, we conducted a thorough search of the literature published before January 5, 2023 (CRD42022357457) to identify observational studies examining the association between dairy product consumption and NAFLD in adult patients (age ≥ 18 years). The following words were combined to find results (Supplementary Table 1): “dairy” or “total dairy” or “dairy product” or “dairy products” or “milk” or “whole milk” or “low-fat milk” or “full-fat milk” or “yogurt” or “yoghurt” or “cream” or “ice cream” or “cheese” or “butter” or “kefir” combined with “fatty liver” or “NAFLD” or “non-alcoholic fatty liver disease” or “hepatocellular cancer” or “hepatic cancer” or “steatohepatitis” or “steatosis” or “nonalcoholic steatohepatitis.” A flowchart of literature selection is presented, in accordance with the Preferred Reporting Items for Meta-Analysis (PRISMA) guidelines (17).
Inclusion and exclusion criteria
De-duplication of identical documents from multiple databases through literature management software such as Endnote. Selection criteria for duplicate literature. (1) Selection of the one with the largest sample size. (2) Selection of the one with the longest follow-up period. (3) Select the one with the most comprehensive study outcomes. The following were the conditions for inclusion: (1) adult population; (2) a study that explored the association between dairy product consumption and the likelihood of developing NAFLD, such as cohort studies, case–control studies or cross-sectional studies; (3) a diagnosis of NAFLD made by ultrasound, magnetic resonance imaging (MRI), controlled attenuation parameter (CAP), fibro-scan, fatty liver index, or liver biopsy; (4) consumption of dairy products: total dairy, milk, yogurt, cheese, or other types of dairy products; (5) outcome was NAFLD; (6) language was restricted to English. Exclusion criteria were as follows: (1) teenaged or pregnant participants; (2) surface antigens for hepatitis B, antibodies against hepatitis C, or HIV antibodies present; (3) abnormally high alcohol or drug intake that could be hazardous to the liver (tamoxifen, steroids, and amiodarone); and (4) reviews, comments, editorials, letters, interviews, or reports.
Data extraction and quality assessment
From each study, the following information was extracted: first author, country, publication year, study design, sample size, number of cases, body mass index (BMI), participants’ mean age, NAFLD diagnostic method, dietary assessment tools, types of exposure, risk estimate (HRs, RRs, or ORs and its 95% CI), and confounding factors adjusted in the final model. The Newcastle-Ottawa scale (18) and the Agency for Healthcare Research and Quality (19) were used to assess the quality of cohort studies, case–control studies, and cross-sectional studies. The Newcastle-Ottawa scale was used to rate the literature quality with a score out of 9 stars, with higher scores indicating higher quality studies; scores of ≥ 6 and < 6 indicated high- and low-quality studies, respectively. Scores of 0–3, 4–7 and 8–11 on the Agency for Healthcare Research and Quality indicated low-, moderate- and high-quality literature, respectively.
Statistical analysis
The RRs and HRs used in this meta-analysis were assumed to be roughly equivalent to ORs. Heterogeneity was assessed using the I2 statistic (20), and I2 > 50% indicated a high degree of heterogeneity between the studies. Depending on the degree of heterogeneity, we either used fixed-effects or random-effects models to construct ORs and 95% CIs. (I2 < 50, fixed-effects model; I2 ≥ 50, random-effects model). After excluding each article from the overall analysis, a sensitivity analysis was conducted to determine how each article contributed to the overall composite result. To evaluate publication bias, Egger’s and Begg’s tests were used (21, 22). p < 0.05 was regarded as possibly biased due to publication.
In the subgroup analysis, the following factors were stratified: (1) study design (cross-sectional or case–control); (2) dietary assessment tools [food frequency questionnaire (FFQ) or dietary recall]; (3) regions (Europe or Asia); (4) sex (men or women); (5) BMI (18.5–24.9 kg/m2, ≥ 25 kg/m2, or ≥ 30 kg/m2); (6) types of exposure (milk, yogurt, cheese, or ice cream); and (7) NAFLD diagnostic criteria (CAP, ultrasonography, MRI, or NAFLD-related scores). Meta-regression analysis was conducted to determine possible associations between the above factors. Stata 17.0 software (Stata Corp, College Station, TX, United States) was used for the statistical analysis. In addition, the p value was two-tailed, with a value < 0.05 considered statistically significant.
Results
Literature search
A flowchart depicting the study selection process is shown in Figure 1. According to PubMed, Web of Science, and Scopus, 4,634 articles were identified. We excluded 310 articles that contained duplicate content and 3,812 articles for which the titles and abstracts did not match. The full text of the remaining 512 articles were read, and 498 were excluded because they were animal studies (n = 385), reviews or editorials (n = 101), or their data could not be extracted (n = 12). Ultimately, 14 studies (including seven cross-sectional studies, one cohort study and six case–control studies), including 25 estimates, met the inclusion criteria.
Study characteristics
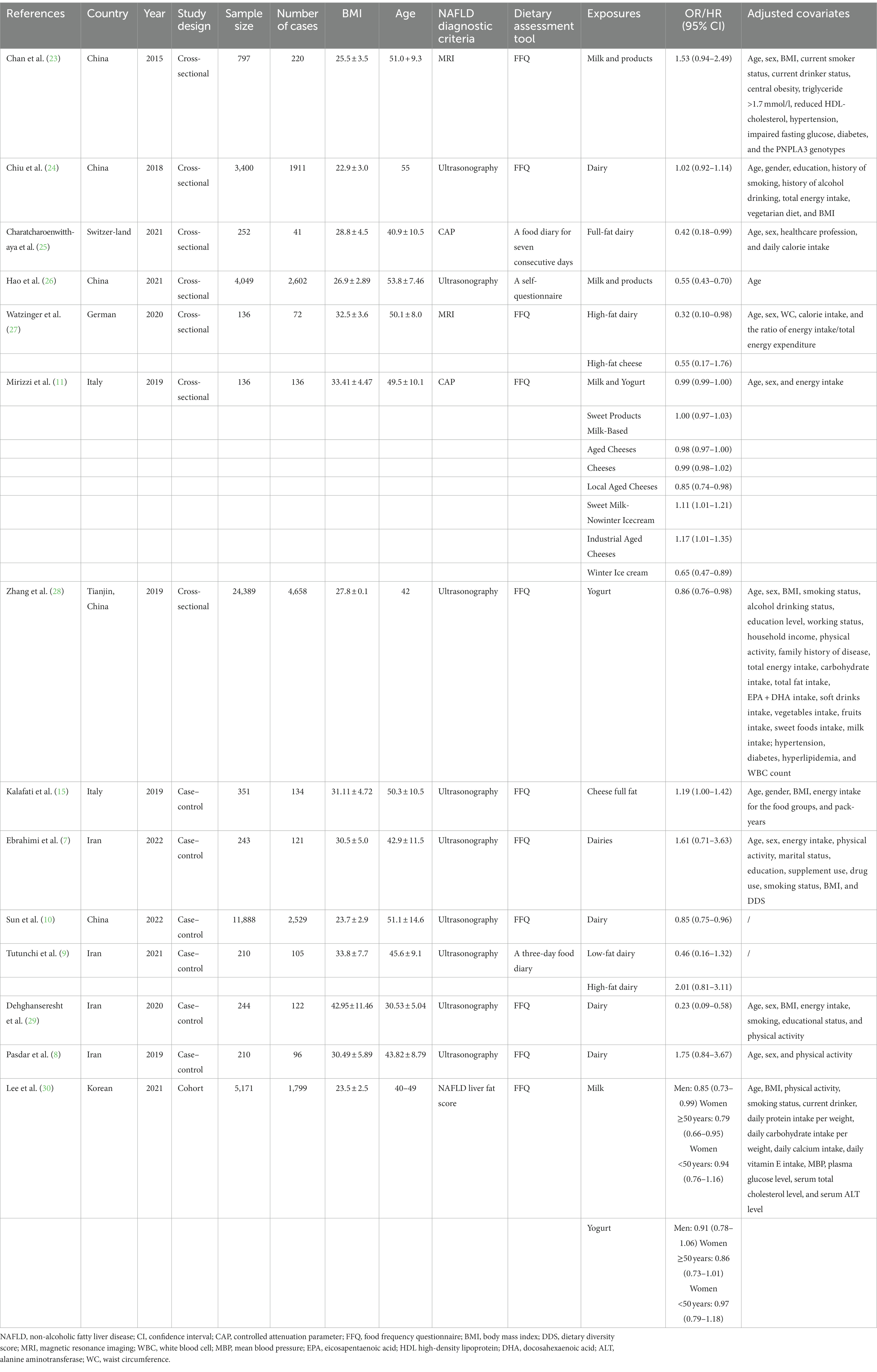
Table 1 summarizes the characteristics of the study. The inclusion criteria were met by a total of 14 studies with 51,476 participants (33,159 in seven cross-sectional studies, 5,171 in one cohort study and 13,146 in six case–control studies) and 14,546 cases of NAFLD (9,640 in seven cross-sectional studies, 1,799 in one cohort study and 3,107 in six case–control studies). There was a wide range of publication years, ranging from 2015 to 2022. Among them, four studies were from Europe and nine from Asia. The results were divided into different subgroups based on exposure type, including milk, yogurt, cheese, and ice cream.
The calibration of the included studies is reported in Supplementary Tables 2 and 3. All studies were of appropriate quality, based on two scales. The quality scores of the cohort studies and case–control studies ranged from seven to eight, while those of the cross-sectional studies ranged from seven to nine.
Association between dairy products consumption and NAFLD
In total, 14 articles (including 25 effect groups) investigated the associations between the consumption of dairy products and NAFLD; the results of the pooled analysis are shown in Figure 2. The forest plot showed that dairy product consumption was associated with a lower likelihood of NAFLD (OR = 0.97, 95% CI = 0.94–0.99).
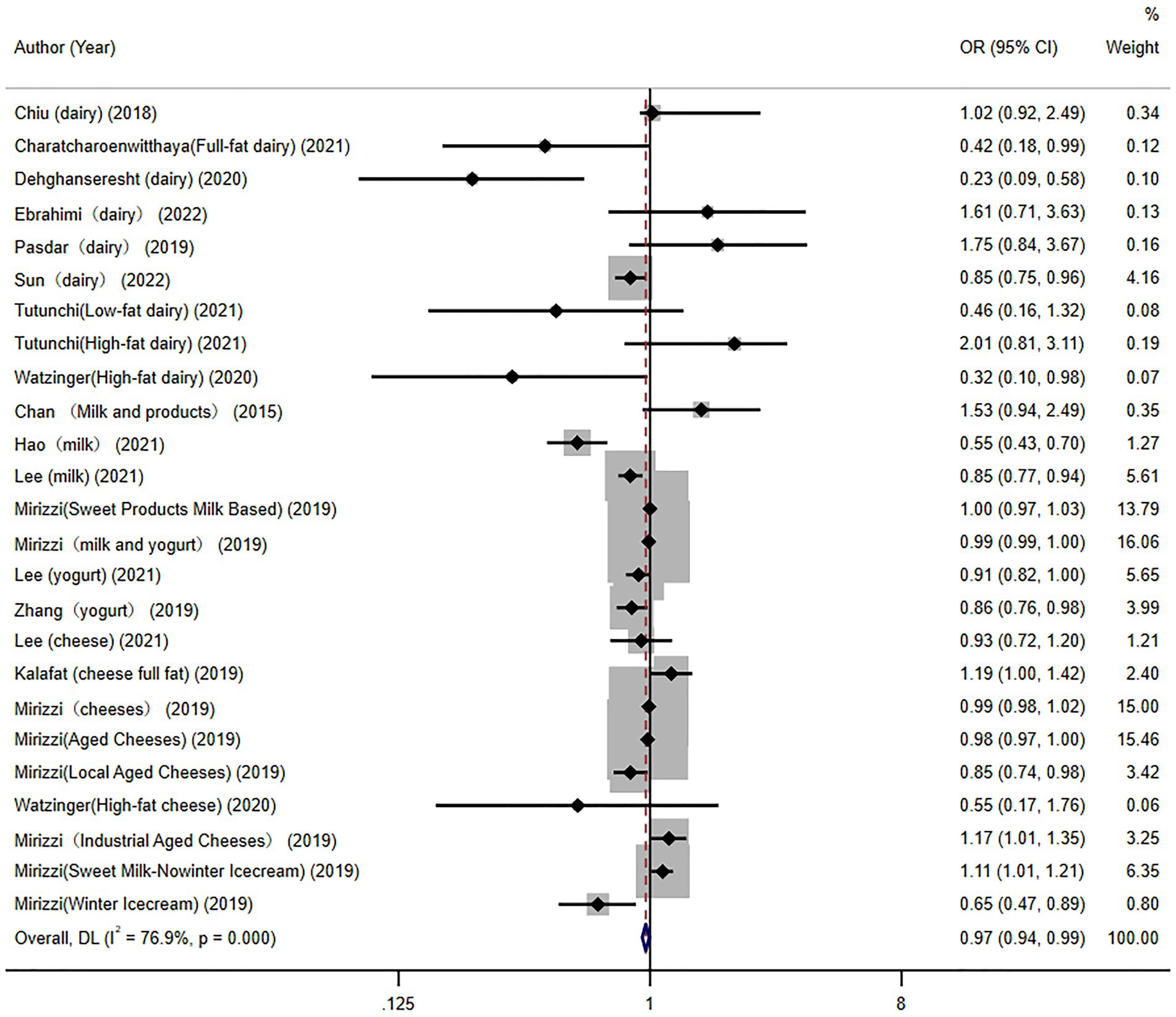
Figure 2. Overall pooled analysis of association between dairy products and non-alcoholic fatty liver disease.
Subgroup analysis
Several subgroup analysis were also performed (Table 2). In accordance with, we divided the patients into two subgroups according to the design of each study (cross-sectional and case–control). The cross-sectional studies (OR = 0.98, 95% CI = 0.96–1.01) and case–control studies (OR = 1.02, 95% CI = 0.73–1.42) showed no significant association between dairy product consumption and NAFLD. Subgroup analysis stratified by sex demonstrated that dairy product consumption was associated with a lower likelihood of NAFLD (OR = 0.98, 95% CI = 0.95–0.99) in women, but not in men (OR = 0.83, 95% CI = 0.40–1.72). Subgroup analysis stratified by BMI demonstrated that dairy product consumption was associated with a lower likelihood of NAFLD in patients with a BMI of 18.5–24.9 kg/m2 (OR = 0.88, 95% CI = 0.83–0.93), but not in patients with a BMI ≥ 25 kg/m2 (OR = 0.78, 95% CI = 0.52–1.16) and a BMI ≥ 30 kg/m2 (OR = 1.00, 95% CI = 0.97–1.02). Based on the type of exposure, we divided all studies into four subgroups (milk, yogurt, cheese, or ice cream). The yogurt consumption (OR = 0.89, 95% CI = 0.82–0.96) and milk consumption (OR = 0.94, 95% CI = 0.87–1.00) was associated with a lower likelihood of NAFLD. However, cheese (OR = 0.99, 95% CI = 0.96–1.03), and ice cream (OR = 0.87, 95% CI = 0.52–1.47) were not associated with NAFLD. Subgroup analysis stratified by exposure assessment showed that consumption of dairy products assessed using FFQ was inversely associated with NAFLD (OR = 0.97, 95% CI = 0.94–0.99), while no significant association was found when exposure was assessed using dietary recall (OR = 0.76, 95% CI = 0.25–2.29). Subgroup analysis stratified by study region showed that dairy product intake was associated with a lower likelihood of NAFLD in Asian populations (OR = 0.90, 95% CI = 0.77–0.97), but not in European populations (OR = 0.99, 95% CI = 0.97–1.01). Finally, subgroup analysis stratified by assessments of NAFLD showed that dairy product intake was inversely associated with NAFLD when NAFLD-related scores (OR = 0.88, 95% CI = 0.83–0.95) were used; however, no significant association was found when NAFLD was assessed using ultrasonography (OR = 0.91, 95% CI = 0.73–1.13), MRI (OR = 0.72, 95% CI = 0.26–2.02), and CAP (OR = 0.99, 95% CI = 0.97–1.01).
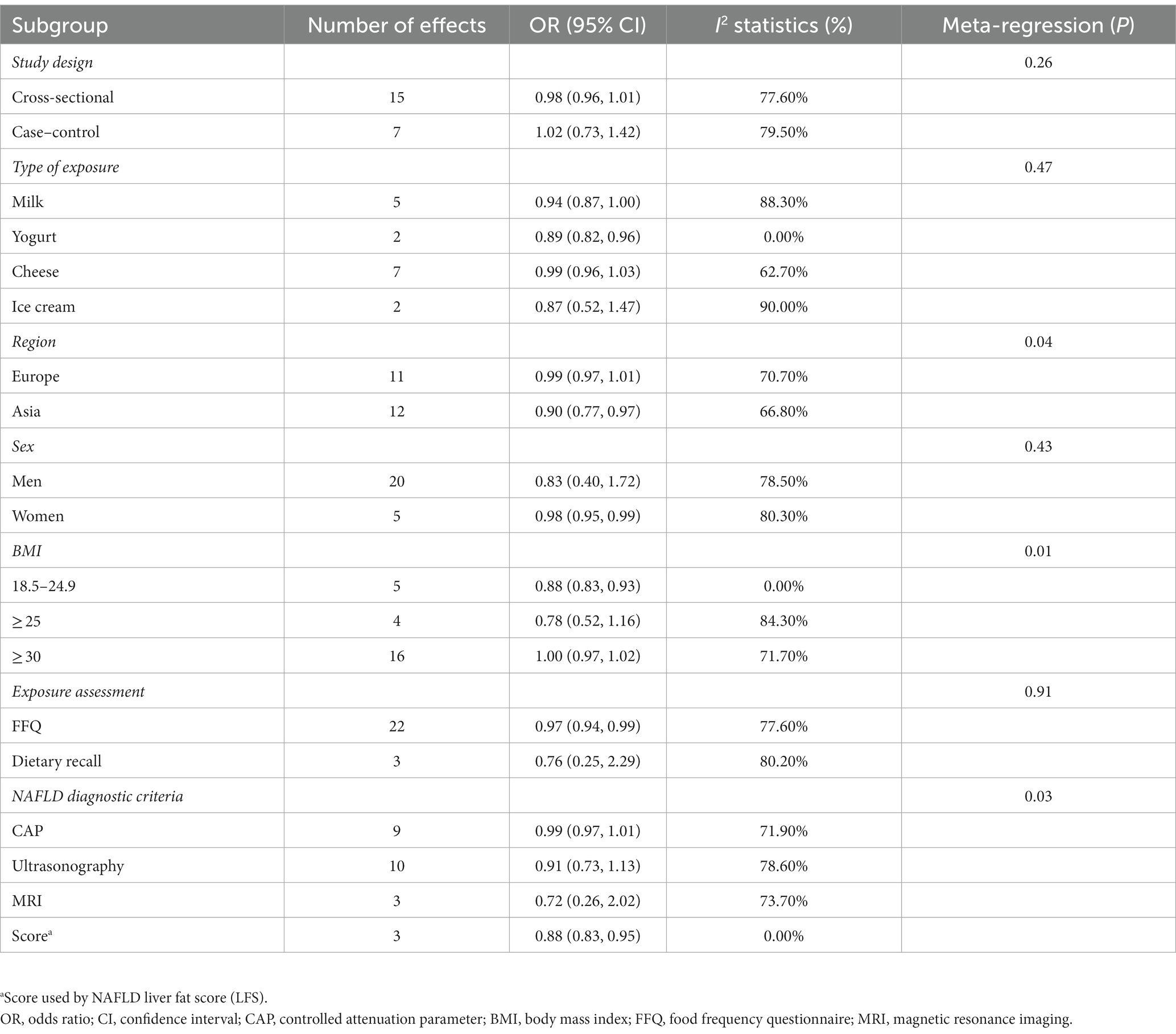
Table 2. A subgroup analysis of the association between dairy product consumption and non-alcoholic fatty liver disease (NAFLD).
Sensitivity analysis and meta-regression
When successive articles were excluded from the sensitivity analysis, the results remained unchanged (Supplementary Figure 1). Meta-regression analysis (Table 2) showed that study design (p = 0.26), type of exposure (p = 0.47), sex (p = 0.43), and exposure assessment (p = 0.91) were not associated with heterogeneity, while region, NAFLD diagnostic criteria and BMI had a significant effect on heterogeneity (p < 0.05).
Publication bias
Publication bias was evaluated using Egger’s test (p > 0.05), Begg’s test (p > 0.05), and funnel plots (Supplementary Figure 2), and these analysis revealed no publication bias.
Discussion
The results showed that a lower likelihood of NAFLD was associated with dairy product consumption. However, when the types of dairy products were categorized, yogurt consumption and milk consumption were found to be significant among the factors associated with a lower likelihood of NAFLD. Subgroup analysis suggested that dairy product consumption was linked to a lower likelihood of NAFLD in subgroups of Asian populations, women, patients diagnosed using NAFLD-related scores, patients with a BMI of 18.5–24.9 kg/m2, and dairy product intake assessment using FFQ. In contrast, no significant associations were observed in the other subgroups. To explore possible sources of (expected) heterogeneity in the studies, we performed subgroup and meta-regression analysis, used sensitivity analysis to check the robustness of the results, and measured publication bias. Significant heterogeneity was present in most analysis, and this significant heterogeneity may reflect differences in the characteristics of the study population (region and BMI) and in the diagnostic approach to NAFLD. In a previous study, European populations were identified as a possible source of heterogeneity (31), which may be related to regional differences in the inclusion of participants. In addition, there were other factors such as study design and sample size that may also affect heterogeneity.
A previous study evaluated the association between dairy product intake and NAFLD (16), finding no significant correlation in cross-sectional studies. However, based on the results of case–control studies, dairy consumption was found to be positively associated with NAFLD. Despite this, as a result of the small sample size, the results of this previous study were limited. Moreover, the associations between dairy products and NAFLD in the different subgroups were not explored. Therefore, it was not possible to conclude from this previous study that dairy products caused NAFLD in a comprehensive manner. In this study, compared to previous meta-analysis, firstly, we conducted an updated search with more stringent inclusion criteria; whereas the previous meta-analysis was conducted in 2019, we conducted a thorough search for literature published before 5 January 2023. Secondly, ten additional articles were included in comparison to the previous article. Third, we included a more comprehensive range of dairy product types (e.g., ice cream) Fourth, we performed subgroup analysis and meta-regression based on study design, region, sex, BMI, type of exposure, NAFLD diagnostic criteria and exposure assessment tools. Fifth, we also performed a sensitivity analysis simultaneously. An analysis of 96 patients revealed that low-fat dairy intake was negatively correlated with NAFLD (32), a finding supported by a prospective cohort study of 101,510 Chinese participants demonstrating lower likelihood of NAFLD risk among consumers of dairy products (10). Several possible mechanisms could explain why dairy product intake is negatively associated with NAFLD. First, dairy products offer crucial dietary micronutrients such as calcium, iron, and vitamins. (33). A higher intake of dairy products may help prevent skeletal sarcopenia, an established risk factor for NAFLD (34). Second, diabetes-related insulin resistance is a major cause of NAFLD. An epidemiological study showed that dairy intake is negatively correlated with insulin resistance (35). Third, dairy consumption, particularly low-fat dairy products, had positive benefits on insulin resistance, waist circumference, and body weight, according to a recent meta-analysis (36), which was beneficial for NAFLD.
Our results found a negative association between yoghurt consumption and NAFLD. In line with our findings, a cross-sectional study of 24,389 adults found that participants who consumed yoghurt more than four times a week were less likely to develop NAFLD. Other similar studies have shown that yogurt consumption may have a preventive role in the development of other chronic diseases (28). The following aspects may partially explain the observed results. First, probiotics are abundant in yogurt. Probiotics may prevent the onset of NAFLD by inhibiting the lipopolysaccharide and hepatic toll-like receptor 4 signaling pathway, according to animal studies (37). Second, previous research has shown that probiotics from yogurt have anti-inflammatory, antioxidant, and immune-modulating properties, which may explain why people who consume more yogurt have a reduced prevalence of NAFLD (38, 39). Finally, yogurt is one of the most nutrient-dense foods and is high in proteins, vitamins, and minerals (such as calcium, magnesium, and potassium). There is proof that consuming more calcium, which is present in yogurt, results in more fat being burned throughout the body (40).
Furthermore, our study found that dairy product intake was inversely associated with NAFLD in Asian but not European populations, which may be due to differences in the epidemiological features of NAFLD and the dairy consumption habits = in different regions. For example, cheese, which has a high saturated fatty acid content, is much more popular in European populations than in Asian populations. We also found a clear positive correlation between dairy intake and NAFLD in women, but not in men. Previous studies (41) have shown that dairy product consumption was more protective against NAFLD in women than in men. This may be because estradiol exerts a protective effect against liver injury by inhibiting lipid accumulation and liver fibrosis (42). Lifestyle changed, including dietary habits and physical activity, should be the first line of treatment for NAFLD. Dietary modification therefore played a key role, as diets rich in carbohydrates, especially those high in fructose, were a major cause of obesity, insulin resistance and the development of NAFLD (43). Following the Mediterranean diet can reduce liver fat, even without weight loss, and it is the most recommended dietary pattern for NAFLD. The Mediterranean diet is characterized by a reduced intake of carbohydrates, especially sugar and refined carbohydrates, and an increased intake of monounsaturated and omega-3 fatty acids (44). The Mediterranean diet has also been found to improve metabolism and lower the risk of diabetes (45) and cardiovascular disease (46), two outcomes that are closely associated in people with NAFLD.
This study had several advantages. First, we conducted a comprehensive systematic search and applied comprehensive subgroup analysis to assess the associations between dairy consumption, including that of various dairy products, and NAFLD. Second, sensitivity and meta-regression analysis were performed to check the robustness of the results and explore potential heterogeneity.
However, the study also had several limitations. First, few articles were included in this study, and data on American populations were especially lacking. Second, all the included studies were observational, which has inherent limitations; for example, causality was uncertain. Third, the majority of patients with NAFLD in the included studies were diagnosed using ultrasonography, which is not the gold standard diagnostic method. However, liver biopsy is only performed when clinically indicated and is neither practical nor ethical for large epidemiological studies. Fourth, doogh is an important dairy product in parts of Asia, but we found no evidence for it in the available evidence, so further research is needed to explore this topic.
Conclusion
In conclusion, a lower likelihood of NAFLD was associated with dairy product consumption, particularly milk consumption and yogurt consumption. Consumption of dairy products could help prevent the development of non-alcoholic fatty liver disease. However, given the few studies included, the results need further confirmation by more cohort studies and randomized controlled trials.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding authors.
Author contributions
WD and HL: conceptualization, formal analysis, visualization, and writing—original draft. TZ, QC, YZ, and CG: writing—review and editing. YX: conceptualization, resources, writing—review and editing, supervision, and funding acquisition. All authors contributed to the article and approved the submitted version.
Funding
This study was supported by the National Natural Science Foundation of China (grant number: 81903302), the Young Elite Scientists Sponsorship Program by China Association for Science and Technology (grant number: YESS20200151), and the 345 Talent Project of ShengJing Hospital of China Medical University (grant number: M0294).
Acknowledgments
We are grateful to all the participants of the study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnut.2023.1119118/full#supplementary-material
Abbreviations
NAFLD, non-alcoholic fatty liver disease; CIs, confidence intervals; ORs, odds ratios; RRs, relative risks; BMI, body mass index; CAP, controlled attenuation parameter; FFQ, food frequency questionnaire; MRI, magnetic resonance imaging.
References
1. Vernon, G, Baranova, A, and Younossi, ZM. Systematic review: the epidemiology and natural history of non-alcoholic fatty liver disease and non-alcoholic steatohepatitis in adults. Aliment Pharmacol Ther. (2011) 34:274–85. doi: 10.1111/j.1365-2036.2011.04724.x
2. Anderson, EL, Howe, LD, Jones, HE, Higgins, JP, Lawlor, DA, and Fraser, A. The prevalence of non-alcoholic fatty liver disease in children and adolescents: a systematic review and meta-analysis. PLoS One. (2015) 10:e0140908. doi: 10.1371/journal.pone.0140908
3. Younossi, ZM, Koenig, AB, Abdelatif, D, Fazel, Y, Henry, L, and Wymer, M. Global epidemiology of nonalcoholic fatty liver disease-meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology. (2016) 64:73–84. doi: 10.1002/hep.28431
4. Friedman, SL, Neuschwander-Tetri, BA, Rinella, M, and Sanyal, AJ. Mechanisms of NAFLD development and therapeutic strategies. Nat Med. (2018) 24:908–22. doi: 10.1038/s41591-018-0104-9
5. Abenavoli, L, Di Renzo, L, Boccuto, L, Alwardat, N, Gratteri, S, and De Lorenzo, A. Health benefits of Mediterranean diet in nonalcoholic fatty liver disease. Expert Rev Gastroenterol Hepatol. (2018) 12:873–81. doi: 10.1080/17474124.2018.1503947
6. Ratajczak, AE, Zawada, A, Rychter, AM, Dobrowolska, A, and Krela-Kaźmierczak, I. Milk and dairy products: good or bad for human bone? Practical dietary recommendations for the prevention and Management of Osteoporosis. Nutrients. (2021) 13:1329. doi: 10.3390/nu13041329
7. Ebrahimi Mousavi, S, Dehghanseresht, N, Dashti, F, Khazaei, Y, Salamat, S, Asbaghi, O, et al. The association between dietary diversity score and odds of nonalcoholic fatty liver disease: a case-control study. Eur J Gastroenterol Hepatol. (2022) 34:678–85. doi: 10.1097/MEG.0000000000002344
8. Pasdar, Y, Moradi, S, Moludi, J, Darbandi, M, Niazi, P, Nachvak, SM, et al. Risk of metabolic syndrome in non-alcoholic fatty liver disease patients. Mediterr J Nutr Metab. (2019) 12:353–63. doi: 10.3233/MNM-190290
9. Tutunchi, H, Saghafi-Asl, M, Asghari-Jafarabadi, M, and Ostadrahimi, A. Association between dietary patterns and non-alcoholic fatty liver disease: results from a case-control study. Arch Iran Med. (2021) 24:35–42. doi: 10.34172/aim.2021.06
10. Sun, Y, Chen, S, Zhao, X, Wang, Y, Lan, Y, Jiang, X, et al. Adherence to the dietary approaches to stop hypertension diet and non-alcoholic fatty liver disease. Liver Int. (2022) 42:809–19. doi: 10.1111/liv.15156
11. Mirizzi, A, Franco, I, Leone, CM, Bonfiglio, C, Cozzolongo, R, Notarnicola, M, et al. Effects of some food components on non-alcoholic fatty liver disease severity: results from a cross-sectional study. Nutrients. (2019) 11:2744. doi: 10.3390/nu11112744
12. Hirahatake, KM, Bruno, RS, Bolling, BW, Blesso, C, Alexander, LM, and Adams, SH. Dairy foods and dairy fats: new perspectives on pathways implicated in Cardiometabolic health. Adv Nutr. (2020) 11:266–79. doi: 10.1093/advances/nmz105
13. Canfora, EE, Jocken, JW, and Blaak, EE. Short-chain fatty acids in control of body weight and insulin sensitivity. Nat Rev Endocrinol. (2015) 11:577–91. doi: 10.1038/nrendo.2015.128
14. Kratz, M, Marcovina, S, Nelson, JE, Yeh, MM, Kowdley, KV, Callahan, HS, et al. Dairy fat intake is associated with glucose tolerance, hepatic and systemic insulin sensitivity, and liver fat but not β-cell function in humans. Am J Clin Nutr. (2014) 99:1385–96. doi: 10.3945/ajcn.113.075457
15. Kalafati, IP, Dimitriou, M, Borsa, D, Vlachogiannakos, J, Revenas, K, Kokkinos, A, et al. Fish intake interacts with TM6SF2 gene variant to affect NAFLD risk: results of a case-control study. Eur J Nutr. (2019) 58:1463–73. doi: 10.1007/s00394-018-1675-4
16. He, K, Li, Y, Guo, X, Zhong, L, and Tang, S. Food groups and the likelihood of non-alcoholic fatty liver disease: a systematic review and meta-analysis. Br J Nutr. (2020) 124:1–13. doi: 10.1017/S0007114520000914
17. Moher, D, Liberati, A, Tetzlaff, J, and Altman, DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. (2009) 6:e1000097. doi: 10.1371/journal.pmed.1000097
18. Stang, A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. (2010) 25:603–5. doi: 10.1007/s10654-010-9491-z
19. Hu, J, Dong, Y, Chen, X, Liu, Y, Ma, D, Liu, X, et al. Prevalence of suicide attempts among Chinese adolescents: a meta-analysis of cross-sectional studies. Compr Psychiatry. (2015) 61:78–89. doi: 10.1016/j.comppsych.2015.05.001
20. Higgins, JP, Thompson, SG, Deeks, JJ, and Altman, DG. Measuring inconsistency in meta-analyses. BMJ. (2003) 327:557–60. doi: 10.1136/bmj.327.7414.557
21. Egger, M, Davey Smith, G, Schneider, M, and Minder, C. Bias in meta-analysis detected by a simple, graphical test. BMJ. (1997) 315:629–34. doi: 10.1136/bmj.315.7109.629
22. Begg, CB, and Mazumdar, M. Operating characteristics of a rank correlation test for publication bias. Biometrics. (1994) 50:1088–101. doi: 10.2307/2533446
23. Chan, R, Wong, VW, Chu, WC, Wong, GL, Li, LS, Leung, J, et al. Diet-quality scores and prevalence of nonalcoholic fatty liver disease: a population study using proton-magnetic resonance spectroscopy. PLoS One. (2015) 10:e0139310. doi: 10.1371/journal.pone.0139310
24. Chiu, TH, Lin, MN, Pan, WH, Chen, YC, and Lin, CL. Vegetarian diet, food substitution, and nonalcoholic fatty liver. Ci Ji Yi Xue Za Zhi. (2018) 30:102–9. doi: 10.4103/tcmj.tcmj_109_17
25. Charatcharoenwitthaya, P, Tansakul, E, Chaiyasoot, K, Bandidniyamanon, W, and Charatcharoenwitthaya, N. Dietary composition and its association with newly diagnosed nonalcoholic fatty liver disease and insulin resistance. Nutrients. (2021) 13. doi: 10.3390/nu13124438
26. Hao, X, Ma, C, Xiang, T, Ou, L, and Zeng, Q. Associations among methylene tetrahydrofolate reductase rs1801133 C677T gene variant, food groups, and non-alcoholic fatty liver disease risk in the Chinese population. Front Genet. (2021) 12:568398. doi: 10.3389/fgene.2021.568398
27. Watzinger, C, Nonnenmacher, T, Grafetstätter, M, Sowah, SA, Ulrich, CM, Kauczor, HU, et al. Dietary factors in relation to liver fat content: a cross-sectional study. Nutrients. (2020) 12. doi: 10.3390/nu12030825
28. Zhang, S, Fu, J, Zhang, Q, Liu, L, Lu, M, Meng, G, et al. Association between habitual yogurt consumption and newly diagnosed non-alcoholic fatty liver disease. Eur J Clin Nutr. (2020) 74:491–499. doi: 10.1038/s41430-019-0497-7
29. Dehghanseresht, N, Jafarirad, S, Alavinejad, SP, and Mansoori, A. Association of the dietary patterns with the risk of non-alcoholic fatty liver disease among Iranian population: a case-control study. Nutr J. (2020) 19:63. doi: 10.1186/s12937-020-00580-6
30. Lee, JH, Lee, HS, Ahn, SB, and Kwon, YJ. Dairy protein intake is inversely related to development of non-alcoholic fatty liver disease. Clin Nutr. (2021) 40:5252–60. doi: 10.1016/j.clnu.2021.08.012
31. Vos, B, Moreno, C, Nagy, N, Féry, F, Cnop, M, Vereerstraeten, P, et al. Lean non-alcoholic fatty liver disease (lean-NAFLD): a major cause of cryptogenic liver disease. Acta Gastroenterol Belg. (2011) 74:389–94.
32. Ferolla, SM, Ferrari, TC, Lima, ML, Reis, TO, Tavares, WC Jr, Couto, OF, et al. Dietary patterns in Brazilian patients with nonalcoholic fatty liver disease: a cross-sectional study. Clinics (São Paulo). (2013) 68:11–7. doi: 10.6061/clinics/2013(01)OA03
33. Tunick, MH, and Van Hekken, DL. Dairy products and health: recent insights. J Agric Food Chem. (2015) 63:9381–8. doi: 10.1021/jf5042454
34. Wijarnpreecha, K, Panjawatanan, P, Thongprayoon, C, Jaruvongvanich, V, and Ungprasert, P. Sarcopenia and risk of nonalcoholic fatty liver disease: a meta-analysis. Saudi J Gastroenterol. (2018) 24:12–7. doi: 10.4103/sjg.SJG_237_17
35. Pereira, MA, Jacobs, DR Jr, Van Horn, L, Slattery, ML, Kartashov, AI, and Ludwig, DS. Dairy consumption, obesity, and the insulin resistance syndrome in young adults: the CARDIA study. JAMA. (2002) 287:2081–2089. doi: 10.1001/jama.287.16.2081
36. Sochol, KM, Johns, TS, Buttar, RS, Randhawa, L, Sanchez, E, Gal, M, et al. The effects of dairy intake on insulin resistance: a systematic review and meta-analysis of randomized clinical trials. Nutrients. (2019) 11. doi: 10.3390/nu11092237
37. Xue, L, He, J, Gao, N, Lu, X, Li, M, Wu, X, et al. Probiotics may delay the progression of nonalcoholic fatty liver disease by restoring the gut microbiota structure and improving intestinal endotoxemia. Sci Rep. (2017) 7:45176. doi: 10.1038/srep45176
38. Maddur, H, and Neuschwander-Tetri, BA. More evidence that probiotics may have a role in treating fatty liver disease. Am J Clin Nutr. (2014) 99:425–6. doi: 10.3945/ajcn.113.082636
39. Eslamparast, T, Poustchi, H, Zamani, F, Sharafkhah, M, Malekzadeh, R, and Hekmatdoost, A. Synbiotic supplementation in nonalcoholic fatty liver disease: a randomized, double-blind, placebo-controlled pilot study. Am J Clin Nutr. (2014) 99:535–42. doi: 10.3945/ajcn.113.068890
40. Zemel, MB. Proposed role of calcium and dairy food components in weight management and metabolic health. Phys Sportsmed. (2009) 37:29–39. doi: 10.3810/psm.2009.06.1707
41. Keshavarz, Z, Rahimlou, M, Farjam, M, Homayounfar, R, Khodadost, M, Abdollahi, A, et al. Non-alcoholic fatty liver disease and dairy products consumption: results from FASA Persian cohort study. Front Nutr. (2022) 9:962834. doi: 10.3389/fnut.2022.962834
42. Lee, C, Kim, J, and Jung, Y. Potential therapeutic application of estrogen in gender disparity of nonalcoholic fatty liver disease/nonalcoholic steatohepatitis. Cells. (2019) 8:1259. doi: 10.3390/cells8101259
43. Lange, NF, Radu, P, and Dufour, JF. Prevention of NAFLD-associated HCC: role of lifestyle and chemoprevention. J Hepatol. (2021) 75:1217–27. doi: 10.1016/j.jhep.2021.07.025
44. Romero-Gómez, M, Zelber-Sagi, S, and Trenell, M. Treatment of NAFLD with diet, physical activity and exercise. J Hepatol. (2017) 67:829–846. doi: 10.1016/j.jhep.2017.05.016
45. Salas-Salvadó, J, Bulló, M, Estruch, R, Ros, E, Covas, MI, Ibarrola-Jurado, N, et al. Prevention of diabetes with Mediterranean diets: a subgroup analysis of a randomized trial. Ann Intern Med. (2014) 160:1–10. doi: 10.7326/M13-1725
Keywords: milk, non-alcoholic fatty liver disease, dairy, meta-analysis, systematic review
Citation: Dai W, Liu H, Zhang T, Chang Q, Zhao Y, Guo C and Xia Y (2023) Dairy product consumption was associated with a lower likelihood of non-alcoholic fatty liver disease: A systematic review and meta-analysis. Front. Nutr. 10:1119118. doi: 10.3389/fnut.2023.1119118
Edited by:
Roberta Zupo, National Institute of Gastroenterology S. de Bellis Research Hospital (IRCCS), ItalyReviewed by:
Mohammad Hassan Sohouli, Shahid Beheshti University of Medical Sciences, IranAmmar Salehi, Shahid Beheshti University of Medical Sciences, Iran
Copyright © 2023 Dai, Liu, Zhang, Chang, Zhao, Guo and Xia. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Chuanji Guo, ✉ guocj@sj-hospital.org; Yang Xia, ✉ xytmu507@126.com
†These authors have contributed equally to this work
 Wei Dai1,2†
Wei Dai1,2†  Qing Chang
Qing Chang Chuanji Guo
Chuanji Guo Yang Xia
Yang Xia