Abstract
Context:
Many nursing educational approaches have been applied on patients with heart failure (HF) to improve their outcomes. The results of these approaches on outcomes of patients with HF remain controversial.Evidence Acquisition:
The aim of this study was to highlight the importance of nursing education to improve the outcomes of patients with HF, such as self-care behaviour, quality of life, mortality, readmission and hospitalization rates. A systematic review was conducted in the MEDLINE database on investigations punished from 2000 to 2012. The search terms used were self-care, heart failure, nursing, and education. A total of 22 studies complied with the eligibility criteria for this review.Results:
The findings of the reviewed studies showed that self-care behaviour of patients who received nursing education improved significantly. No significant improvement was noticed in the health-related quality of life. Additionally, there was no significant reduction in readmission, hospitalization and mortality rates of patients after implementing this educational process.Conclusions:
The effectiveness of nursing education on self-care behaviour of HF patients was clearly demonstrated. Methodological differences in development and implementation of education programs, made the comparison between the results of the studies difficult.Keywords
Heart Failure Nursing Education Nursing Teaching Patient Outcomes Quality of Life Self-Care
1. Context
Heart failure (HF) is a chronic and progressive clinical syndrome. Treatment of HF requires application of complex clinical interventions and regimens. HF is characterized by a number of symptoms due to inability of the heart to eject adequate amount of blood to peripheral tissues to meet their metabolic needs. This results to limited functional capacity of patients and experienced symptoms such as fatigue, limited tolerance, weakness, shortness of breath, fluid retention and swelling (1).
According to the annual epidemiological data of the American heart association, approximately five million persons in the United States live with HF and more than 550000 new cases are diagnosed annually. The incidence of HF in people over the age of 65 years is 10% of the population. These rates seem to double every decade. HF is the most frequent cause of hospitalization among patients over 65 years and it is characterized by high mortality rates (50% of patients with HF in an advanced stage would die during the next year) (2).
It is commonly accepted that management of HF depends significantly on patient. Many studies, however, argue that patients are unable to manage the effects of disease adequately and do not adapt to the newly imposed but appropriate lifestyle (3-6).
Despite progress on pharmacological regimens for the treatment of HF, professionals on cardiology and cardiovascular nursing demonstrate the necessity of multidisciplinary management programs. Besides integrated approach in the management of HF, patient education is an essential component of nursing care and aims to improve the ability of patients to take care of themselves (7).
An important element in the treatment of HF is self-care, which is based on strategy decisions made by patient alone or together with his or her family, so as to cope with the disease and maintain functionality and well-being (8). The promotion of self-care is achieved through education, which aims to improve knowledge of HF and enhance special skills in patients (9). Through properly designed educational process, patients are required to adopt their new daily life habits regarding medication, diet, exercise, smoking, prevention of infections, monitoring disease symptoms and seeking medical help when dangerous symptoms appear (10, 11).
Studies and meta-analyses supported the effectiveness of education to improve knowledge about HF among patients (12), their ability to cope with the disease and to improve their self-care behaviour to reduce the cost of health care by reduced hospitalization rates and days of hospitalization (13-15).
Nurses play an essential role on patient compliance with the recommended regimen and effective disease management. Nurses are asked to provide appropriate information and encourage patients to make decisions on disease self-management.
Education is an ethical and legal obligation of nursing. Implementation of education for patients with HF may be an important and independent nursing intervention, as well as an effective nursing tool for improving patient’s self-care behaviour (16-18).
Considering all the above, the aim of this study was to systematically review and highlight the importance of nursing education to improve outcomes of patients with HF such as self-care behaviour, health related quality of life, mortality, readmission and hospitalization rates.
2. Evidence Acquisition
2.1. Search Method
A systematic review was conducted in the current literature on publications regarding effectiveness of nursing education on outcomes of patients with HF such as self-care behaviour, health-related quality of life, readmissions, hospitalization, and mortality rates. This review was performed to answer the following research questions: To determine self-care behaviour in patients with HF after implementation of an education program by nurses and to evaluate the effectiveness of nursing education in reducing mortality, hospitalization and readmission rates and improving the quality of life of patients with HF.
Two of the authors performed independently a systematic literature review in September 2013. This review was conducted using the US national library of medicine, PubMed interface on published investigations from 2000 to 2012. Used keywords were self-care, heart failure, nursing, teaching, outcomes, quality of life, readmissions, hospitalization and education. Only English articles were included.
2.2. Type of Studies and Type of Participants
Retrieved articles were originally selected for more detailed evaluation. References lists of each study were also checked to identify manually additional studies that could answer the research question.
For the study selection, the study population was previously determined and inclusion and exclusion criteria were defined. Inpatients and outpatients with HF, stages I to IV by the NYHA, adults ≥ 18 years old, regardless of their gender, who attended nursing educational programs constituted the study population.
Self-care behaviour was assessed before and after implementation of education program. Studies were evaluated, as well as, readmission rates due to HF, hospitalization rates due to HF, mortality rates and quality of life.
2.3. Types of Educational Programs
Patients’ education was performed by nurses. Random clinical studies, in which education was performed in different ways (using brochure, CD, groups meetings, via telephone or follow-up visits), were taken into consideration. To evaluate self-care behaviour and quality of life, valid and reliable measurement instruments were used.
2.4. Outcomes
Eligible studies for our systematic review were those that investigated the effect of nursing education on the following outcomes of patients with HF; self-care behaviour, health-related quality of life, mortality, readmission and hospitalization rates.
2.5. Exclusion Criteria
Following studies were excluded; studies that assessed the views of nurses or families of patients with HF about how to conduct self-care, studies in which patients’ education was performed by any other health professional rather than a nurse, and finally qualitative studies in which self-care behaviour and quality of life were not evaluated with reliable quantitative instruments.
3. Results
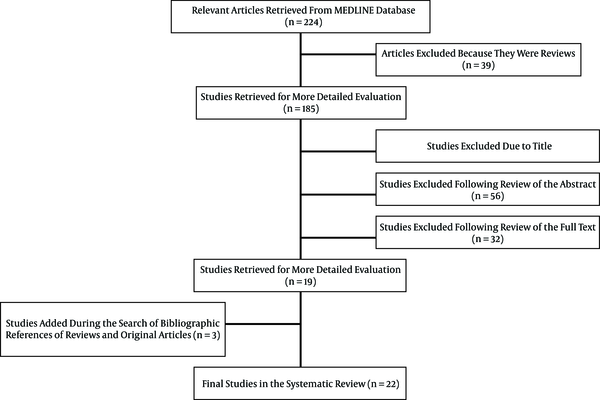
Figure 1 demonstrates and the steps of selecting eligible studies. A list of the exact number of studies evaluated and selected or rejected at every step is also included. Seven studies were retrieved from the bibliographic references of reviewed studies and other reviews. Finally, 22 original studies complied with the quality criteria that could answer the research question were included in review (12, 14, 16-35).
Selection Flowchart
Tables 1 - 5 summarizes the main characteristics of 22 selected studies. Severity of HF was determined using the NYHA classification. In about 50% of studies, patients who participated in education programs were in II to IV stages (12, 14, 19, 22, 24, 26, 31, 32, 34, 35), while in four studies patients were evaluated in the first stage (17, 18, 20, 30). Only in 32% of studies, the severity of HF was not assessed (16, 21, 23, 25, 27, 28, 33).
Main Characteristics of the Studies Included in the Systematic Review
| References | Intervention | Instruments | Outcomes | Study Population |
|---|---|---|---|---|
| Yehle et al. 2009 (16) | 1-hour semi structured education on HF for patients and one family member, the education was provided by a nurse practitioner and the primary investigator. participants in the control group saw the nurse practitioner for a one-on-one 30-minute visit. follow-up period: 8 weeks | Self-Care heart failure index (SCHFI) | Self-Care | n = 23; control group, (n = 10); intervention group, (n = 13); male, 59%; mean age, 67.3 |
| Lupon et al. 2008 (17) | Nursing intervention with face to face education with leaflets for patients and their families, and with posters in the waiting room about signs of worsening heart failure. Follow-up period: one year | European heart failure self-care behaviour scale (EHFScBS) | Self-Care | n = 151; no control group; male, 111; mean age, 65.4; NYHA, I-IV |
| Shearer et al. 2007 (18) | Nursing intervention with standardized education written and verbal information concerning HF from a staff nurse, and viewing an educational video about HF. telephone-delivered EI by telephone 1 to 3 days after discharge, follow-up period: 2, 4, 6, 8 and 12 weeks | SF-36, Self-management of heart failure scale (SMHF) | Self-management, quality of life | n = 90; intervention group (n = 45); control group (n = 45); male, 56; mean age, 76.03; NYHA: I-IV |
| Holst et al. 2007 (19) | Nursing intervention consisted of education and counseling in the home including written, verbal and interactive educational material and a multimedia program on CD-ROM, follow-up period: 3 and 12 months | European heart failure self-care behaviour scale (EHFScBS), EQ-5D | Self-care, quality of life | n = 78; no control group; male, 31; mean age, 79; NYHA: II-IV |
| Sisk et al. 2006 (20) | Nurse-led intervention focused on specific management problems, follow-up period: 2, 4, 8, 12 and 24 weeks | Short form-12 (SF-12), Minnesota living with heart failure questionnaire (MLHF) | Hospitalization rates, readmission rates, quality of life, mortality rates | n = 406; intervention group (n = 203); control group (n = 203); male: 53.7 %; mean age, 59.4; NYHA: I-IV |
Main Characteristics of the Studies Included in the Systematic Review
| Author | Intervention | Instruments | Outcomes | Study Population |
|---|---|---|---|---|
| Domingues et al. 2011 (21) | Eight calls per patient during a three month period aiming at clarifying and reinforcing instructions received during hospitalization and monitoring signs and symptoms of decompensation and investigating possible visits to the emergency care unit and rehospitalisation | readmission rates, rehospitalisation rates, mortality rates | n = 84; intervention group (n = 38), control group (n = 44); mean age, 63 ± 13; male: 64NYHA: II-IV | |
| Riegel et al. 2006 (22) | Nursing intervention with telephone case management standardized using a decision-support software program-at home with heart failure, follow-up period: 1, 3 and 6 months | Minnesota living with HF questionnaire, EQ-5D, patient health questionnaire | Hospitalization rates, readmission rates, quality of life, mortality rates | n = 134; intervention group (n = 69); control group (n = 65); female, 72% ; mean age, 72.1; NYHA:II-IV |
| Stromberg et al. 2006 (23) | Nursing intervention in nurse-led HF clinics with standard education and computer-based education through an interactive multimedia program on CD-ROM, follow-up period: 1 and 6 months | EQ-5D, Minnesota living with HF questionnaire, cardiac health profile | Quality of life | n = 154; intervention group (n = 82); control group (n = 72); male, 54% and 55%; mean age, 70 |
| Blue et al. 2001 (24) | Nursing intervention consisted of a number of planned home visits and were given a pocket sized booklet containing an explanation of HF and its treatment, follow-up period: 2, 4, 6, 8, 10 and 12 months | Readmission rates, mortality rates | n = 165; intervention group (n = 82); control group (n = 75); mean age, 75.6(7.9) and 74.4(8.6); male, 41 and 54; NYHA: IΙ-IV |
Main Characteristics of the Studies Included in the Systematic Review
| Author | Intervention | Instruments | Outcomes | Study Population |
|---|---|---|---|---|
| Caldwell et al. 2005 (25) | Individualized nursing education and counseling session using a portable, standardized, high-impact, colored flip chart conducted in the physician’s office or patient’s home, control group received usual care and written material, follow-up period: 3 months | European heart failure self-care behaviour scale (EHFScBS) | Self-care | n = 36; intervention group (n = 20); control group (n =1 6); mean age:71; male:69% |
| Martensson et al. 2005 (26) | Nurse-led intervention program consisted of one extensive session including education and counseling, provided in the home of the patient including written, verbal and interactive information and a multimedia program on CD-ROM provided on a laptop computer, follow-up period: 3 and 12 months | SF-36, Minnesota living with heart failure questionnaire (MLWHF), Zung Self-rating, depression scale (SDS) | Quality of life | n = 153; intervention group (n = 78); control group (n = 75); mean age:79; male:83; NYHA: II-IV |
| Koelling et al. 2005 (27) | Nursing intervention with a patient education program including a 60-minute, one on one teaching session with a nurse educator before discharge, follow-up period: 30, 90 and 180 days | Minnesota living with heart failure questionnaire [MLHF] | Hospitalization rates, quality of life Mortality rates, self-care | n = 223; intervention group (n = 107); control group (n = 116); mean age: 65 and 64.7; female: 42/group |
| Scott et al. 2004 (28) | Three specific nursing interventions were used in a home visit during the first week of client’s admission to agency’s care, follow-up: 3 and 6 months | Mental health inventory-5 (MHI-5), cardiac version of the quality of life index, (QLI) | Quality of life | n = 88; 3 intervention group mutual goal setting (n = 27) supportive educative (n = 28); placebo(n = 33); mean age: 75/group; male:42%, 50% - 41% |
Main Characteristics of the Studies Included in the Systematic Review
| Author | Intervention | Instruments | Outcomes | Study Population |
|---|---|---|---|---|
| Kimmelsti et al. 2004 (29) | A nurse-manager conducted a home visit, meeting with the patient and the respective spouse/partner/caregiver. Each visit lasted 45 to 90 minutes. Patients and family received a pre-printed Patient and Family Handbook, follow-up period: 3 and 12 months | Hospitalization rates | n = 200; intervention group (n = 97); control group (n = 103); mean age: 70.3, 73.9; Female: 42.3% - 41.7%; NYHA: II-III | |
| LaFramboise et al. 2003 (30) | Four groups received educational content of the HF disease management program, which differed between groups in the method of delivery and number of in home contacts. Two groups received assessment and education through a tele health communication device called the health buddy, follow-up period: 2 months | Short Form-36, (SF-36) | Quality of Life | n = 90; 4 intervention groups (n1 = 26, n2 = 23, n3 = 21, n4 = 20), male: 50%; mean age: 70,3 |
| Stromberg 2003 (31) | Nursing education about HF and social support to the patient and his family at a nurse-led heart failure clinic, 2 - 3 weeks after discharge. Follow-up period: 3 and 12 months | European heart failure self-care behaviour scale (EHFScBS) | Mortality rates; readmission rates; Self-care | n = 106; intervention group (n = 52); control group (n = 54); mean age: 77 ± 7 and 78 ± 6; male: 65; NYHA: II-IV |
| Riegel et al. 2002 (14) | Telephonic case management by a registered nurse was provided using a decision support software program. follow-up period: 3 and 6 months | Readmission rates; hospitalization rates | n = 358; intervention group (n = 130); control group (n = 228); mean Age: 72.52 ± 13.05; and 74.63 ± 12; male: 175; NYHA: II-IV |
Main Characteristics of the Studies Included in the Systematic Review
| Author | Intervention | Instruments | Outcomes | Study Population |
|---|---|---|---|---|
| Jaarsma et al. 2000 (12) | Education by a study nurse in 4 visits in the hospital, 1 telephone call and 1 home visit, follow-up period: 1, 3 and 9 months | Heart failure self-care behaviour scale, appraisal of self-care agency (asa) scale, hf functional status inventory psychosocial adjustment to illness scale (PAIS), Cantril’s Ladder, (ladder of life) | Selfcare, quality of life | n = 132; intervention group (n = 58); control group (n = 74); mean age: 72 ± 9; male: 60%; NYHA: IIΙ-IV |
| Sethares et al. 2004 (32) | Patients received a tailored message intervention by the same research nurse during hospitalization and 1 week and 1 month after hospital discharge, control group received usual care, which included discharge teaching by a staff nurse on the unit and written educational sheets, follow-up period: 1 week, 1 and 3 months | Minnesota living with heart failure, questionnaire (MLHF) | Readmission rates, quality of life | n = 70; intervention group (n = 33); control group (n = 37); mean age: 75.70 ± 12.25 and 76.84 ± 10.48; male: 33; NYHA: IΙ-IV |
| Krumholz et al. 2002 (33) | Experienced cardiac nurse educated patients within two weeks of hospital discharge using a teaching booklet, home visits were performed for 45% of intervention patients unable to attend the hospital, researches contacted patients by phone on a weekly basis for four weeks, then biweekly for eight weeks and then monthly for a total intervention period of one year, patients assigned to the control group received all usual care treatments and services ordered by their physicians, follow-up period: 1 year | Readmission rates, mortality rates | n = 88; intervention group (n = 44); control group (n = 44); mean age: 74; male: 57% | |
| Agren et al. 2012 (34) | Intervention was delivered in 3 sessions through nurse-led face-to-face counseling, a computer-based CD-ROM program and written materials, all sessions were conducted in home or in the heart failure clinic in a 12-week period, control group received care as usual, including traditional care in hospital and outpatient education and support | European heart failure self-care behaviour scale (EHFscBS), short form (SF)-36 | Selfcare, quality of life | n = 155; intervention group (n = 71); control group (n = 84); mean age: 70 ± 10 and 67 ± 12; male: 19.1% and 30.9%; NYHA: II-IV |
| Aguado et al. 2010 (35) | The intervention consisted of a home visit by a nurse to patients 1 week after discharge, educational session centered on self-management, habits, and preventive activities, control group did not participate at an educational program, follow up period: 6 months, 5 and 24 months | Specific Minnesota living with heart failure questionnaire (MLWHFQ), short form-36 (SF-36) | Readmission rates, rehospitalisation rates, mortality, quality of life | n = 106 intervention group (n = 42); control group (n = 64); mean age: 77.8 ± 5.8 and 77.4 ± 6.8; male: 76.2% and 65.6% |
The studies evaluated the impact of education programs provided by nurses on improvement of self-care behaviour in patients with HF and on achieved clinical outcomes such as improvement of quality of life and reduction of mortality, readmission and hospitalization rates due to HF because of deregulation of HF.
3.1. Nursing Educational Approaches
The content of the education in the reviewed studies included patient compliance with medication, diet, exercise, vaccination program and recognition of symptoms and their management. Each study differed regarding organization of education programs, the time the educational process took place (during hospitalization in the outpatient clinic or at home) and educational methods (educational booklets, CD-ROMs, videos).
3.2. Studies Design
In total, 82% of studies contained experimental (intervention) and control groups (12, 14, 16, 18, 20-27, 29, 31-35). In two trials, comparisons were made between intervention groups with different education programs (28, 30) and two studies had no control group at all (17, 19).
3.3. Self-Care Behaviour
In all studies, nursing education was evaluated after follow-up education programs over 2 weeks to 24 months. From the studies that met the inclusion criteria, nine were designed to assess self-care behaviour of patients with H (12, 16-19, 25, 27, 31, 34). In each study, different measurement tools were used, so it was impossible to aggregate data. Eight studies used valid instruments specifically designed to assess self-care behavior (12, 16-19, 25, 31, 34). In the study of Koelling et al. (27), evaluation of self-care behaviour was conducted by investigating the application of self-care practices such as recording weight, exercise and smoking cessation. Implementation of educational programs was found to be effective on improving self-care behaviour in patients with HF at seven of nine studies. No statistically significant difference was found in studies of Holst et al. (19), Agren et al. (34), Lupon et al. (17), trying to investigate the effects of education on self-care behaviour without the use of a control group, a fact that limits significantly reliability of these studies.
3.4. Health-Related Quality of Life
The impact of nursing education on health-related quality of life in patients with HF was examined in thirteen studies (12, 18-20, 22, 23, 26-28, 30, 32, 34, 35). In these studies, different tools for assessing quality of life were used. In five (20, 22, 23, 26, 35) of thirteen studies, two different tools were used, a specific tool for assessing the quality of life for patients with HF and a general assessment instrument. Only two studies (20, 28) found improvement on quality of life of patients after implementation of an educational program, while nine studies (12, 19, 22, 23, 26, 27, 32, 34, 35) found no statistically significant difference after their participation in such programs. LaFramboise et al. (30) highlighted that quality of life had a significant change in four subscales of the SF-36 such as role physical, mental health, bodily pain and vitality. In the study of Shearer et al. (18), there was no improvement related to physical dimension, but higher scores were found on mental aspect of patients with HF.
3.5. Mortality
Eight studies assessed mortality rates in patients who attended an educational program for HF management (20-22, 24, 27, 31, 33, 35) (Table 6). Five studies reported their results as relative risk ratio (RR) (20, 24, 27, 33, 35), two as proportion (21, 22) and one as a cumulative risk (31). In most studies, no significant decrease in mortality rates was found for patients who received nursing education with RR between 0.69 and 0.94. Stromberg (31) found a significant difference in the number of deaths in the intervention group (P = 0.005). Riegel et al. (22) found no significant difference in mortality rates, though mortality was low overall to be estimated.
Outcomes of Studies Included in This Systematic Review
| Study | Mortality Rates | All-Cause Readmission Rates | Readmission Rates Due to HF | All-cause Hospitalization Rates | Hospitalization Rates Due to HF |
|---|---|---|---|---|---|
| Sisk et al. 2006 (20) | RR 0.88 [0.48, 1.61], 95% CI | Cumulative readmissions, -10% change, -0.05 (-0.23, 0.12) 12 - 18 months, 95% CI | - | Cumulative hospitalizations, -37% change, -0.19 (-0.38, -0.01) 12 months and -18% change, -0.20 (-0.46, 0.05) 12 - 18 months, 95% CI | Cumulative hospitalizations, -0.14 (-0.23, -0.04), 95% CI |
| Koelling et al. 2005 (27) | RR 0.94 (0.34, 2.6), P = 0.91, 95% CI | - | - | - | RR 0.49(0.27, 0.88), P = 0.015, 95% CI |
| Stromberg 2003 (31) | Cumulative risk, intervention group: 13%, control group: 37% | 82 vs. 92, P = 0.31 | - | - | - |
| Krumholz et al. 2002 (33) | RR 0.69 (0.33, 1.45), P = 0.33, 95% CI | -38.8% change, P = 0.06 | -47.6 change, P = 0.07 | - | - |
| Blue et al. 2001 (24) | RR 0.93 (0.54, 1.63), P = 0.8195% CI | RR 0.71(0.54, 0.94), P = 0.018, 95% CI | 0.40(0.23, 0.71), P = 0.000495% CI | - | - |
| Riegel et al. 2006 (22) | 25% lower (intervention group) | 58% proportion admitted for HF at least once (intervention group), 56.9%(Usual care), P = 1.0 | 31.9% proportion admitted for HF at least once (intervention group), 33.8% (usual care), P = 0.85 | RR Intervention group 1.06 ± 1.3(0.74, 1.4), usual care, 1.08 ± 1.4(0.75, 1.4) | RR intervention group, 0.55 ± 1.1(0.32, 0.78), usual care, 0.49 ± 0.81(0.25, 0.73) |
| Riegel et al., 2002 (14) | - | RR -13.8% change, P = 0.49 | RR -35.9% change, P = 0.06 | -28.8% change, P = 0.11 | -47.8% change, P = 0.02 |
| Sethares et al. 2004 (32) | - | - | not significantly related to group, P = 0.22 | - | - |
| Kimmelstiel et al. 2004 (29) | - | - | - | RR 1.05, P = 0.70, 95% CI | RR 1.02, P = 0.93, 95% CI |
| Domingues et al. 2011 (21) | RR 0.61 (0.25 to 1.48), (CI 95%), P = 0.38 | RR 0.66 (0.21 to 2.05), (CI 95%), P = 0.67 | - | 1.14 (0.72 to 1.82), (CI 95%), P = 0.72 | - |
| Aguado et al 2010 (35) | Intervention group 46.67%, control group 55.36%, P = 0.448 | Intervention group mean:0.68; control group mean:1.71; P = 0.003 | - | - | - |
3.6. Readmission Rates
Eight studies reported readmission rates after implementation of nursing educational programs (14, 20-22, 24, 31, 33, 35) (Table 6). The follow-up period in each study varied between three (21), six (22, 23) and twelve months (24, 31, 33). One study had twelve to eighteen months (20) and one 24 months follow-up (35). In five of seven studies, no statistically significant difference was found regarding reduction of readmissions between intervention and control groups. Stromberg (31) found that three months after the intervention the number of readmissions reduced by 42% (P = 0.047), however twelve months after implementation of this education program no significant decrease in the rate of readmissions was noticed. Blue et al. (24) found that during one year of follow-up, rates of readmissions of patients with HF decreased with RR 0.71 (0.54, 0.94), P = 0.018. Krumholz et al. (33) found a significant reduction in all-cause readmission rates in the intervention group one year after patient discharge.
Readmission rates due to HF were evaluated in five studies (14, 22, 24, 32, 33) (Table 6), with follow-up after the intervention in three (32), six (14, 22) and twelve months (24, 33). Readmission rates due to HF seemed to decrease significantly in one study (24). Krumholz et al. (33) found that readmission rate after one year of intervention decreased significantly by 47.5%. Patients at the same study had at least one readmission due to deregulation of HF with RR 0.60 (0.41, 0.89), P = 0.01. Stromberg (31) found a significant reduction of HF readmission rates (35.9%) in the intervention group at 6-month follow-up.
3.7. Hospitalization Rates
Five studies assessed the overall hospitalization rates (14, 20-22, 29) and five studies evaluated hospitalization rates due to HF (14, 20, 22, 27, 29) (Table 6). In all studies, no statistically significant results were found in reduction of hospitalization rates for any reason (14, 20-22, 29). In three studies, a statistically significant effect on hospitalization rates due to HF was found (14, 20, 27). Riegel et al. (14) found a statistically significant difference three and six months after the intervention regarding reduction of hospitalization rates due to HF (45.7%, P = 0.03, 47.8%, P = 0.02). Similarly 6 months later, the rates decreased significantly in the study of Koelling et al. with RR 0.49 (0.27 - 0.88), P = 0.015 (27).
Our systematic review highlighted the importance of educational programs in patients with HF as part of their comprehensive treatment. Interpreting the results of 22 reviewed studies, great improvement was noticed on self-care behaviour of patients who received education for effective management of HF. However, there was not a significant reduction on readmission, hospitalization and mortality rates of patients after the educational process. Furthermore, no significant improvement was found on health-related quality of life of patients with HF.
As aforementioned, most reviewed studies demonstrated a significant association between nursing education and promotion of self-care behaviour in HF patients. Through education, HF patients can move from the simple level of self-maintenance to the advanced level of self-management (36). Additionally, targeted educational programs to enhance self-care behaviour could improve outcomes of patients with HF, such as reduction of mortality levels (15).
However, nursing education does not seem to positively affect outcomes of patients with HF such as quality of life, readmission, hospitalization and mortality rates. Inability to draw conclusions about the effectiveness of nursing educational programs in improvement of these outcomes is possibly due to different design of research studies, demographic and clinical characteristics of patients with HF among studies, time tracking, tools used to evaluate examined patient outcomes and educational approaches.
The educational programs used in the reviewed studies differed significantly for strategy implementation (average, duration, time, and manner of implementation) and content. These factors seemed to determine the targeted achievements of each educational program and should be considered when evaluating the results of a study (37).
The study of Stromberg et al. (23) evaluated the impact of nursing education using computers to enhance knowledge about HF and improve quality of life. Researchers argued that this type of education is useful, when there is not an adequate number of health professional to implement these education programs. The effectiveness of using computers in contrast to using leaflets and verbal information was supported by another comparative study in patients with hypertension (38). In addition, other studies claimed that providing video tapes gives an opportunity to patients to receive a greater quantity of complex information about HF (37). Moreover, patient education via telephone improved clinical outcomes, such as reducing readmissions rates. However, such methods should take into account individual characteristics of patients and severity of their clinical status (14).
Furthermore, determinant factors for achieving the goals of education are individual patient’s characteristics such as age, sex, severity of HF, co-morbidity, socio-economic factors, educational level, presence of anxiety and depression (39). Most studies in our review did not assess the impact of such factors.
According to the study of Smeulders et al. (40), patients with an advanced cognitive status seem to benefit more from participation in an education program for HF compared to those with a lower cognitive status. However, the same study showed that high educational level was negatively related to improvement of indicators such as quality of life.
The results of the present review showed that health-related quality of life of patients with HF did not improve significantly after participating in educational process. Education programs included adherence to treatment and identification and management of symptoms and compliance with diet restrictions. However, quality of life is a multifactor concept, with a physical dimension, which is improved by educating patients with HF, as well as psychological and social dimensions, which seem to be affected significantly by presence of disease, but did not constitute a part of education programs as presented by most studies (41).
To achieve effective improvement in all dimensions of quality of life, patient education should be based on a more holistic approach. Factors associated with a poorer quality of life such as social isolation and loss of social function experienced by patients in family and business environment should be taken into account (42, 43). Besides, limited physical function and loss of social roles lead to loss of self-esteem, anxiety, and depression (44, 45).
In the study of Shearer et al. (18), there was no improvement in the sum of scale of physical dimension, but they found higher scores in the mental aspect in patients with HF. This result is likely to accompany the sense of security gained by patients who know how to manage their symptoms.
The results of studies on quality of life are considerably limited as resulted from a variety of measurement tools, which are either specific instruments for heart failure (12, 27, 28, 32), general tools measuring quality of life (18, 19, 30, 34) or both (20, 22, 23, 26, 35). Therefore, sensitivity of tools to enhance quality of life before and after the educational process should be considered.
Sisk et al. (20) found that quality of life in patients with heart failure improved six months after the training process. In this study, the mean age of study population was 59.4 years and participants diagnosed with chronic HF, NYHA classes I-IV. Compared with other studies of the review, where no significant differences were found, individual patient’s characteristics differed in mean age, with a minimum of 70 years and in stage of heart failure as II-IV when symptoms are more intense and would affect the functional capacity of patients and therefore quality of life. This systematic review aimed to identify the effectiveness of education in improving clinical outcomes such as mortality, all-cause hospital readmissions and readmissions due to HF. After evaluating the results of 22 studies, the ability of nursing education to reduce these rates was not clearly demonstrated. These results conflict with those of other reviews that highlight the effectiveness of education in reducing readmissions (40, 46).
Specifically, Jovicic et al. (46) compared the results of six studies and found a statistically significant reduction in all-cause hospital readmissions and readmissions due to HF in patients participated in educational process. In the systematic review of McAlister et al. (15) an interesting methodology was followed; 29 studies were clustered to issue results. More specifically, they found that educational strategies that incorporated a specialized monitoring team led to a reduction in mortality rates (RR 0.75, 95% CI 0.59 - 0.96), hospitalizations rates due to HF (RR 0.74, 95% CI 0.63 to 0.87) and all-cause hospitalization rates (RR 0.81, 95% CI 0.71 to 0.92). Targeted education to enhance patient’s self-care strategies seemed to reduce HF hospitalization rates (RR 0.66, 95% CI 0.52 to 0.83) and all-cause hospitalizations (RR 0.73, 95% CI 0.57 to 0.93), but not mortality rates (RR 1.14, 95% CI, 0.67 to 1.94).
4. Conclusions
From the results of assessed studies in this systematic review, it is not clear whether nursing education has a strong positive effect on outcomes of patients with HF, such as health-related quality of life, mortality rates, all-cause hospital readmission rates and readmission rates due to HF. However, the effectiveness of educational programs in improvement of self-care behaviour of patients with HF is demonstrated. Development of education programs and their implementation require proper planning by a specialized multidisciplinary team. Further research is needed on more appropriate nursing educational programs, which could lead to better HF patient outcomes.
References
-
1.
Hunt SA, Abraham WT, Chin MH, Feldman AM, Francis GS, Ganiats TG, et al. 2009 focused update incorporated into the acc/aha 2005 guidelines for the diagnosis and management of heart failure in adults: A report of the american college of cardiology foundation/american heart association task force on practice guidelines: Developed in collaboration with the international society for heart and lung transplantation. Circulation. 2009;119(14):e391-479. [PubMed ID: 19324966]. https://doi.org/10.1161/CIRCULATIONAHA.109.192065.
-
2.
Heart disease and stroke statistics-2009 update. Dallas, Texas: American Heart Association; 2009.
-
3.
Carlson B, Riegel B, Moser DK. Self-care abilities of patients with heart failure. Heart Lung. 2001;30(5):351-9. [PubMed ID: 11604977]. https://doi.org/10.1067/mhl.2001.118611.
-
4.
Heo S, Moser DK, Lennie TA, Riegel B, Chung ML. Gender differences in and factors related to self-care behaviors: a cross-sectional, correlational study of patients with heart failure. Int J Nurs Stud. 2008;45(12):1807-15. [PubMed ID: 18674762]. https://doi.org/10.1016/j.ijnurstu.2008.05.008.
-
5.
Bentley B, De Jong MJ, Moser DK, Peden AR. Factors related to nonadherence to low sodium diet recommendations in heart failure patients. Eur J Cardiovasc Nurs. 2005;4(4):331-6. [PubMed ID: 15935733]. https://doi.org/10.1016/j.ejcnurse.2005.04.009.
-
6.
Evangelista L, Doering LV, Dracup K, Westlake C, Hamilton M, Fonarow GC. Compliance behaviors of elderly patients with advanced heart failure. J Cardiovasc Nurs. 2003;18(3):197-206. [PubMed ID: 12837010].
-
7.
Tsuyuki RT, Shibata MC, Nilsson C, Hervas-Malo M. Contemporary burden of illness of congestive heart failure in Canada. Can J Cardiol. 2003;19(4):436-8. [PubMed ID: 12704492].
-
8.
Orem DE. Nursing: Concept of practice. 5 ed. Louis: Mosby; 1995.
-
9.
Paul S. Hospital discharge education for patients with heart failure: what really works and what is the evidence? Crit Care Nurse. 2008;28(2):66-82. [PubMed ID: 18378729].
-
10.
Evangelista LS, Shinnick MA. What do we know about adherence and self-care? J Cardiovasc Nurs. 2008;23(3):250-7. [PubMed ID: 18437067]. https://doi.org/10.1097/01.JCN.0000317428.98844.4d.
-
11.
Dracup K, Baker DW, Dunbar SB, Dacey RA, Brooks NH, Johnson JC, et al. Management of heart failure. II. Counseling, education, and lifestyle modifications. JAMA. 1994;272(18):1442-6. [PubMed ID: 7933427].
-
12.
Jaarsma T, Halfens R, Tan F, Abu-Saad HH, Dracup K, Diederiks J. Self-care and quality of life in patients with advanced heart failure: the effect of a supportive educational intervention. Heart Lung. 2000;29(5):319-30. [PubMed ID: 10986526]. https://doi.org/10.1067/mhl.2000.108323.
-
13.
Rich MW, Beckham V, Wittenberg C, Leven CL, Freedland KE, Carney RM. A multidisciplinary intervention to prevent the readmission of elderly patients with congestive heart failure. N Engl J Med. 1995;333(18):1190-5. [PubMed ID: 7565975]. https://doi.org/10.1056/NEJM199511023331806.
-
14.
Riegel B, Carlson B, Kopp Z, LePetri B, Glaser D, Unger A. Effect of a standardized nurse case-management telephone intervention on resource use in patients with chronic heart failure. Arch Intern Med. 2002;162(6):705-12. [PubMed ID: 11911726].
-
15.
McAlister F, Stewart S, Ferrua S, McMurray J. Multidisciplinary strategies for the management of heart failure patients at high risk for admissionA systematic review of randomized trials. J Am Coll Cardiol. 2004;44(4):810-9. https://doi.org/10.1016/s0735-1097(04)01123-4.
-
16.
Yehle KS, Sands LP, Rhynders PA, Newton GD. The effect of shared medical visits on knowledge and self-care in patients with heart failure: a pilot study. Heart Lung. 2009;38(1):25-33. [PubMed ID: 19150528]. https://doi.org/10.1016/j.hrtlng.2008.04.004.
-
17.
Lupon J, Gonzalez B, Mas D, Urrutia A, Arenas M, Domingo M, et al. Patients' self-care improvement with nurse education intervention in Spain assessed by the European Heart Failure Self-Care Behaviour Scale. Eur J Cardiovasc Nurs. 2008;7(1):16-20. [PubMed ID: 17594914]. https://doi.org/10.1016/j.ejcnurse.2007.05.004.
-
18.
Shearer NB, Cisar N, Greenberg EA. A telephone-delivered empowerment intervention with patients diagnosed with heart failure. Heart Lung. 2007;36(3):159-69. [PubMed ID: 17509423]. https://doi.org/10.1016/j.hrtlng.2006.08.006.
-
19.
Holst M, Willenheimer R, Martensson J, Lindholm M, Stromberg A. Telephone follow-up of self-care behaviour after a single session education of patients with heart failure in primary health care. Eur J Cardiovasc Nurs. 2007;6(2):153-9. [PubMed ID: 16928469]. https://doi.org/10.1016/j.ejcnurse.2006.06.006.
-
20.
Sisk JE, Hebert PL, Horowitz CR, McLaughlin MA, Wang JJ, Chassin MR. Effects of nurse management on the quality of heart failure care in minority communities: a randomized trial. Ann Intern Med. 2006;145(4):273-83. [PubMed ID: 16908918].
-
21.
Domingues FB, Clausell N, Aliti GB, Dominguez DR, Rabelo ER. Education and telephone monitoring by nurses of patients with heart failure: randomized clinical trial. Arq Bras Cardiol. 2011;96(3):233-9. [PubMed ID: 21308343].
-
22.
Riegel B, Carlson B, Glaser D, Romero T. Randomized controlled trial of telephone case management in Hispanics of Mexican origin with heart failure. J Card Fail. 2006;12(3):211-9. [PubMed ID: 16624687]. https://doi.org/10.1016/j.cardfail.2006.01.005.
-
23.
Stromberg A, Dahlstrom U, Fridlund B. Computer-based education for patients with chronic heart failure. A randomised, controlled, multicentre trial of the effects on knowledge, compliance and quality of life. Patient Educ Couns. 2006;64(1-3):128-35. [PubMed ID: 16469469]. https://doi.org/10.1016/j.pec.2005.12.007.
-
24.
Blue L, Lang E, McMurray JJ, Davie AP, McDonagh TA, Murdoch DR, et al. Randomised controlled trial of specialist nurse intervention in heart failure. BMJ. 2001;323(7315):715-8. [PubMed ID: 11576977].
-
25.
Caldwell MA, Peters KJ, Dracup KA. A simplified education program improves knowledge, self-care behavior, and disease severity in heart failure patients in rural settings. Am Heart J. 2005;150(5):983. [PubMed ID: 16290977]. https://doi.org/10.1016/j.ahj.2005.08.005.
-
26.
Martensson J, Stromberg A, Dahlstrom U, Karlsson JE, Fridlund B. Patients with heart failure in primary health care: effects of a nurse-led intervention on health-related quality of life and depression. Eur J Heart Fail. 2005;7(3):393-403. [PubMed ID: 15718180]. https://doi.org/10.1016/j.ejheart.2004.01.016.
-
27.
Koelling TM, Johnson ML, Cody RJ, Aaronson KD. Discharge education improves clinical outcomes in patients with chronic heart failure. Circulation. 2005;111(2):179-85. [PubMed ID: 15642765]. https://doi.org/10.1161/01.CIR.0000151811.53450.B8.
-
28.
Scott L, Setterkline K, Britton A. The effects of nursing interventions to enhance mental health and quality of life among individuals with heart failure. App Nurs Res. 2004;17(4):248-56. https://doi.org/10.1016/s0897-1897(04)00074-6.
-
29.
Kimmelstiel C, Levine D, Perry K, Patel AR, Sadaniantz A, Gorham N, et al. Randomized, controlled evaluation of short- and long-term benefits of heart failure disease management within a diverse provider network: the SPAN-CHF trial. Circulation. 2004;110(11):1450-5. [PubMed ID: 15313938]. https://doi.org/10.1161/01.CIR.0000141562.22216.00.
-
30.
LaFramboise LM, Todero CM, Zimmerman L, Agrawal S. Comparison of Health Buddy with traditional approaches to heart failure management. Fam Community Health. 2003;26(4):275-88. [PubMed ID: 14528134].
-
31.
Stromberg A. Nurse-led heart failure clinics improve survival and self-care behaviour in patients with heart failureResults from a prospective, randomised trial. Eur Heart J. 2003;24(11):1014-23. https://doi.org/10.1016/s0195-668x(03)00112-x.
-
32.
Sethares KA, Elliott K. The effect of a tailored message intervention on heart failure readmission rates, quality of life, and benefit and barrier beliefs in persons with heart failure. Heart Lung. 2004;33(4):249-60. [PubMed ID: 15252415].
-
33.
Krumholz HM, Amatruda J, Smith GL, Mattera JA, Roumanis SA, Radford MJ, et al. Randomized trial of an education and support intervention to preventreadmission of patients with heart failure. J Am Coll Cardiol. 2002;39(1):83-9. https://doi.org/10.1016/s0735-1097(01)01699-0.
-
34.
Agren S, Evangelista LS, Hjelm C, Stromberg A. Dyads affected by chronic heart failure: a randomized study evaluating effects of education and psychosocial support to patients with heart failure and their partners. J Card Fail. 2012;18(5):359-66. [PubMed ID: 22555264]. https://doi.org/10.1016/j.cardfail.2012.01.014.
-
35.
Aguado O, Morcillo C, Delas J, Rennie M, Bechich S, Schembari A, et al. Long-term implications of a single home-based educational intervention in patients with heart failure. Heart Lung. 2010;39(6 Suppl):S14-22. [PubMed ID: 20598745]. https://doi.org/10.1016/j.hrtlng.2010.04.010.
-
36.
Riegel B, Moser DK, Anker SD, Appel LJ, Dunbar SB, Grady KL, et al. State of the science: promoting self-care in persons with heart failure: a scientific statement from the American Heart Association. Circulation. 2009;120(12):1141-63. [PubMed ID: 19720935]. https://doi.org/10.1161/CIRCULATIONAHA.109.192628.
-
37.
Yu DS, Thompson DR, Lee DT. Disease management programmes for older people with heart failure: crucial characteristics which improve post-discharge outcomes. Eur Heart J. 2006;27(5):596-612. [PubMed ID: 16299021]. https://doi.org/10.1093/eurheartj/ehi656.
-
38.
Consoli SM, Said MB, Jean J, Menard J, Plouin P, Chatellier G. Benefits of a computer-assisted education program for hypertensive patients compared with standard education tools. Patient Educ Couns. 1995;26(1-3):343-7. https://doi.org/10.1016/0738-3991(95)00747-n.
-
39.
Smith CE, Koehler J, Moore JM, Blanchard E, Ellerbeck E. Testing videotape education for heart failure. Clin Nurs Res. 2005;14(2):191-205. [PubMed ID: 15793275]. https://doi.org/10.1177/1054773804273276.
-
40.
Smeulders ES, van Haastregt JC, Ambergen T, Stoffers HE, Janssen-Boyne JJ, Uszko-Lencer NH, et al. Heart failure patients with a lower educational level and better cognitive status benefit most from a self-management group programme. Patient Educ Couns. 2010;81(2):214-21. [PubMed ID: 20153132]. https://doi.org/10.1016/j.pec.2010.01.003.
-
41.
Bech P. Quality of life measurements in major depression. Eur Psychiat. 1996;11(3):123-6. https://doi.org/10.1016/0924-9338(96)85176-5.
-
42.
Bosworth HB, Steinhauser KE, Orr M, Lindquist JH, Grambow SC, Oddone EZ. Congestive heart failure patients' perceptions of quality of life: the integration of physical and psychosocial factors. Aging Ment Health. 2004;8(1):83-91. [PubMed ID: 14690872]. https://doi.org/10.1080/13607860310001613374.
-
43.
Azevedo A, Bettencourt P, Alvelos M, Martins E, Abreu-Lima C, Hense HW, et al. Health-related quality of life and stages of heart failure. Int J Cardiol. 2008;129(2):238-44. [PubMed ID: 17996315]. https://doi.org/10.1016/j.ijcard.2007.07.091.
-
44.
Bekelman DB, Havranek EP, Becker DM, Kutner JS, Peterson PN, Wittstein IS, et al. Symptoms, depression, and quality of life in patients with heart failure. J Card Fail. 2007;13(8):643-8. [PubMed ID: 17923356]. https://doi.org/10.1016/j.cardfail.2007.05.005.
-
45.
Faller H, Stork S, Schuler M, Schowalter M, Steinbuchel T, Ertl G, et al. Depression and disease severity as predictors of health-related quality of life in patients with chronic heart failure--a structural equation modeling approach. J Card Fail. 2009;15(4):286-92. [PubMed ID: 19398075]. https://doi.org/10.1016/j.cardfail.2008.10.022.
-
46.
Jovicic A, Holroyd-Leduc JM, Straus SE. Effects of self-management intervention on health outcomes of patients with heart failure: a systematic review of randomized controlled trials. BMC Cardiovasc Disord. 2006;6:43. [PubMed ID: 17081306]. https://doi.org/10.1186/1471-2261-6-43.