Published online May 16, 2015. doi: 10.12998/wjcc.v3.i5.462
Peer-review started: May 29, 2014
First decision: August 18, 2014
Revised: November 20, 2014
Accepted: February 10, 2015
Article in press: February 12, 2015
Published online: May 16, 2015
The current case report is related to a male patient with diabetes, obesity [body mass index (BMI) 33], hypertension and recurrence of anemia associated to melena and deep asthenia. M.P., a 60-year-old obese individual, was referred to our department by the primary care unit (PCU) of our hospital for severe anemia (Hemoglobin 6.5 g/dL) associated to episodes of melena and abdominal pain. In the past 5 mo the patient referred to the local hospital 3 times for episodes of melena (hemoglobin levels showed anemia 9.8 g/dL) but the main gastroenterological exams were completely negative (colonoscopy and gastroscopy). The PCU of our Hospital, after stabilization of the main parameters and blood transfusion for the low levels of hemoglobin, referred the patient to gastroenterologists: the patient was subjected to both colonoscopy and gastroscopy that were negative. Due to the condition of acute severe hemorrhage the patient, during the first 3 h from the access to the PCU, was subjected to arteriography that did not reveal any hemorrhagic foci or vascular alterations. The video capsule for the study of the small bowel showed the presence of blood beginning from the third portion of duodenum but deep gastroscopy did not reveal it. The patient was then subjected to double balloon endoscopy that revealed a severe diverticulosis of the small bowel with blood from the diverticula. The entero-tomografia computerizzata confirmed the diagnosis and revealed an extension of the diverticula for almost the entire small bowel (no diverticula in the colon). The patient was subjected to wide spectrum antibiotic therapy with resolution of the symptoms and stabilization of hemoglobin levels. The surgeon suggests no indication to surgery for the wide area involved from the disease and potential high risk of complication due to the high BMI. At home, the patient started a monthly therapy with rifaximin and probiotics associated to mesalazine. At present, after 12 mo from the last episode of hemorrhage, the patient is in good clinical condition, reduced his body weight of about 7 kg and the hemoglobin levels appear in slow progressive increase (last measurement 13.2 g/dL).
Core tip: The current case report adds an additional tool for the treatment of small bowel diverticula. Although the best recognized treatment is represented by surgical approach, the current case demonstrates the possibility of effective treatment by pharmacological approach. The pharmacological approach allows to treat patient with high surgical risk and all patient with contraindication to surgery; moreover the small bowel preservation avoid all the symptoms and signs of malabsorbtion, inevitably occurring after surgery.
- Citation: De Minicis S, Antonini F, Belfiori V, Lo Cascio M, Marraccini B, Piergallini S, Mosca P, Macarri G. Small bowel diverticulitis with severe anemia and abdominal pain. World J Clin Cases 2015; 3(5): 462-465
- URL: https://www.wjgnet.com/2307-8960/full/v3/i5/462.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v3.i5.462
Small bowel diverticulosis is an uncommon pathology and may exist in two different forms: congenital or acquired. The congenital form is represented exclusively by Meckel’s diverticulum, which is a true diverticulum located on the antimesenteric border of the small bowel, to a variable distance from ileo-cecal valve between 40 to 80 cm[1]. Conversely, the acquired forms of the small bowel diverticula are also named false diverticula: they are lesions consisting of mucosa, submucosa, and serosa without a tunica muscularis[2].
Multiple diverticulosis of the jejunum represents an uncommon pathology of the small bowel that is often asymptomatic. An incidence of about 0.5%-2.3% found in small bowel contrast studies and of 0.3%-4.5% found in autopsies have been reported in the literature[3,4].
In a few percentage of case this condition may lead to several and unspecific symptoms such as malabsorption, anemia, chronic abdominal pain and discomfort. Major complications may be characterized by diverticulitis, hemorrhage, obstruction and perforation, which are described in very selected number of cases[5-7].
The management of symptomatic jejunal diverticulosis is a challenge for clinicians. We herein report a case of a 60-year-old man presented at the primary care unit (PCU) of our hospital for acute abdominal pain associated to vomiting and deep asthenia in a patient with diabetes, obesity [body mass index (BMI) 33], hypertension.
M.P., a 60-year-old obese individual, was referred to our department by the PCU of our hospital for severe anemia (Hemoglobin 6.5 g/dL) associated to episodes of melena and abdominal pain.
In the past 5 mo the patient referred to the local hospital 3 times in 5 mo for melena associated to deep asthenia and one episode of lipotimia (hemoglobin levels showed anemia with values respectively of 9.5, 9.1 and 9.8 g/dL); in the described episodes, both colonoscopy and gastroscopy were negative for the identification of blood sources.
At the present, M.P. occurred to the PCU of our hospital for the forth episode of abundant melena associated to abdominal pain and low-pressure levels (100/50 mmHg).
The main laboratories examinations showed a 6.5 g/dL of hemoglobin levels associated to low levels of iron, with no additional alterations.
The patient was transfused with red packed blood cells and the clinical conditions were stabilized. The patient was referred to the gastroenterologist when the main parameters were: cardiac frequency 90, Saturation 97%, PA 110/70 mmHg.
Both Gastroscopy and colonoscopy were completely negative for the presence of lesion potentially involved in bleeding.
During the first 4 h from the access to the PCU, taking into consideration the gastroscopy and colonoscopy previously executed in other hospital, the patient was subjected to arteriography that did not reveal any alteration or potential sources of bleeding.
After adequate preparation, the patient repeated the colonoscopy that showed regular mucosa and no alteration able to justify massive bleeding. The patient performed video-capsule endoscopy examination that revealed the presence of mucosal areas with blood, extended from the upper part of the jejunum for several centimeters, with no other specifications.
In order to better investigate the small bowel, the patient was subjected to double balloon examination that revealed the presence, just down to the Treitz ligament, of a pattern with numerous and giant diverticula of jejunum.
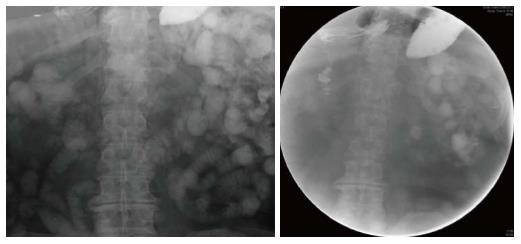
The entero-tomografia computerizzata (TC) and small bowel contrast study (Figure 1) subsequently confirmed the jejunal diverticula, located in the in the right and upper part of the abdomen, apparently related to most of the jejunum; the same diverticula were particularly tick with edema of the mucosal layer, as typical sign of inflammation.
We first referred the case to the surgical department of our Hospital for evaluation: but no criteria for emergency procedures were present, since no active bleeding was occurring at that time; on the other hand, the high number of comorbidities strongly contraindicated any potential surgical procedure.
Due to this analysis and the hemodynamic condition of stability, we decided to start treatment with rifaximine (1200 mg/die), probiotics and mesalazine (1600 mg/die); with the objective to use at home a monthly-based therapy characterized by 1 wk of rifaximine and probiotics and 2 wk of mesalazine.
No additional episodes of bleeding occurred, with a progressive increase of hemoglobin; the patient was discharged after 12 d with no major complications.
At the present, after 12 mo of follow-up, no additional episodes of bleeding occurred, the level of hemoglobin reached 13.2 g/dL and no episodes of abdominal pain were referred. The patient continues treatment with rifaximine, probiotics and mesalazine on a monthly base.
Jejunal diverticulosis was described for the first time by Somerlingin 1794 and by Sir Astley Cooper in 1807. These false diverticula are commonly located on the mesenteric border of the jejunum[8]. The main feature that jejuna diverticula shares with colonic diverticula is that mucosal herniation occur through gaps in the muscle layers[9].
Regarding the portion of the bowel interested by the pathology: Jejunal diverticula may be the only site in the gastrointestinal tract or being associated to colonic diverticula (35%), duodenal diverticula (26%) and esophageal diverticula (2%)[7,8]. Small bowel diverticula are more frequent in male and its prevalence increases in elderly[10].
The low prevalence and the poor symptoms described in the clinical practice may lead to misdiagnosis, or relatively delayed-diagnosis[11].
In the specific clinical case reported in this manuscript, the patient was deeply studied and carefully evaluated with second level examinations only at the forth access to the PCU and only in the condition of severe anemia (hemoglobin 6.5 g/dL) and probably active bleeding. Furthermore, the condition of bleeding necessarily bring the attention to the endoscopic evaluation of the intestinal tract, such as gastroscopy and colonoscopy, that may delayed the time of diagnosis without solving the main problem.
In the specific case the TC imaging analysis was performed only in a condition of hemodynamic stabilization of the patient and overall secondarily to the double-balloon endoscopic examination. The evidence-based flow chart presumably leads to a different approach in the general management of the pathology: in hemodynamically stable patient, endoscopic techniques (gastroscopy or colonoscopy) may be used. Secondarily, small bowel contrast studies and computed tomography scans are able to visualize such regions and thus establish the diagnosis[12]. In our case we preferred to directly perform the double balloon instead of waiting for the radiologic imaging techniques.
As reported in literature, hemorrhage from jejunal diverticula generally presents as lower gastrointestinal bleeding that may be acute or chronic with iron deficiency anemia noted[13].
Although the treatment of choice in bleeding is represented by surgical resection of the source of bleeding with primary anastomoses, the case report described had several contraindication for surgical approach: first, the history of cardiopathy and the low rate of pulmonary reservoir; second, the obesity that greatly limits the feasibility of the technical procedure; third, the lack of a specifically localized source of bleeding, that do not allow to perform a selective resection of the bowel, but may lead to the resection of a too large portion of the bowel[14].
Due to the high number of contraindications to the surgical approach, we decided proposing the patient for pharmacologic treatment.
The drugs used mainly consist in the same protocol existing for the colonic diverticula, characterized by rifaximine, probiotics, and mesalazine cyclically, on a monthly-based therapy.
To date, no exhaustive data are provided in literature on the efficacy of the current used pharmacological therapy and no study of comparison between potential pharmacological therapy and surgical treatment are otherwise described[15]. Furthermore, it is important to take into consideration the high surgical risk due to several comorbidities occurring in this specific patient. Surgeon of our department presented to the patient the potential effect of the surgical therapy and the possibility to obtain a complete resolution of the pathology informing the patient on the main risks of the procedure. In the specific case, the patient refused to perform additional examinations and expressed the clear choice of non-surgical treatment.
Both rifaximine and mesalazine represent an off-label therapy in the specific case of small bowel diverticula and no study, as far as we know, are present in literature discussing this issue[16].
In conclusion, in the general management of small bowel diverticula, acutely showing complication such as hemorrhages, the treatment of choice should be considered the surgical procedure with the resection of the tract of intestine affected by the bleeding[17]. However, it is important to take into consideration two major points occurring in this patient: active bleeding with anemia without the possibility to specifically localize the source of bleeding; second, the presence of major contraindications to surgery[18].
The current case report describe a single patient that referred to the hospital with a severe anemia in the course of acute intestinal bleeding from small bowel diverticula, with no indications to surgery. In the specific case report, the patient referred to the PCU 4 times in the time lap of 8 mo. At the current state, the last acute episode of bleeding was observed 12 mo ago, the hemoglobin levels are progressively increasing (last value was 13.2 g/dL) only with oral administration of iron.
Thus, in the flow chart of therapeutic opportunities for patients with small bowel diverticula, even with previous complication of bleeding, pharmacological therapy option should be considered, especially in the presence of major contraindications for surgical procedures.
Patient develops sever anemia and abdominal pain.
Double-balloon endoscopy revealed the presence of small bowel diverticula.
Signs and symptoms may suggest all the different conditions of upper gastrointestinal (GI) bleeding.
Low hemoglobin levels represent the main sign.
Double balloon endoscopy and radiographic GI imaging revealed the presence of diverticula.
Melena and anemia represent the main features of the clinical case.
Mesalazine and wide spectrum antibiotics.
The majority of case report of complicated small bowel diverticula suggests the resolution of the pathological condition by surgical approach.
The pharmacological treatment in complicated small bowel diverticula should be considered as a treatment option in addition to surgical approach, particularly in those patients that present absolute contraindication or high risk to surgery.
It is comprehensive and elaborating.
P- Reviewer: Mukherjee S, Refaat R S- Editor: Ji FF L- Editor: A E- Editor: Lu YJ
| 1. | Akhrass R, Yaffe MB, Fischer C, Ponsky J, Shuck JM. Small-bowel diverticulosis: perceptions and reality. J Am Coll Surg. 1997;184:383-388. [PubMed] [Cited in This Article: ] |
| 2. | Chow DC, Babaian M, Taubin HL. Jejunoileal diverticula. Gastroenterologist. 1997;5:78-84. [PubMed] [Cited in This Article: ] |
| 3. | Prost A La Denise J, Douard R, Berger A, Cugnenc PH. Small bowel diverticulosis complicated by perforated jejunal diverticula: conservative and/or surgical management? Hepatogastroenterology. 1997;55:1657-1659. [PubMed] [Cited in This Article: ] |
| 4. | Wild JR, Shiwani MH, Ullah Q. Jejunal diverticulitis. J Coll Physicians Surg Pak. 2009;19:120-122. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 1] [Reference Citation Analysis (0)] |
| 5. | Kassahun WT, Fangmann J, Harms J, Bartels M, Hauss J. Complicated small-bowel diverticulosis: a case report and review of the literature. World J Gastroenterol. 2007;13:2240-2242. [PubMed] [Cited in This Article: ] |
| 6. | Shanmugam RP, Shivakumar P. A rare complication of jejunal diverticulosis. Trop Gastroenterol. 2006;27:134-135. [PubMed] [Cited in This Article: ] |
| 7. | Assenza M, Ricci G, Antoniozzi A, Clementi I, Simonelli L, Modini C. Perforated jejuneal diverticulosis. Case report and review of literature. Ann Ital Chir. 2007;78:247-250. [PubMed] [Cited in This Article: ] |
| 8. | Woods K, Williams E, Melvin W, Sharp K. Acquired jejunoileal diverticulosis and its complications: a review of the literature. Am Surg. 2008;74:849-854. [PubMed] [Cited in This Article: ] |
| 9. | Cunningham SC, Gannon CJ, Napolitano LM. Small-bowel diverticulosis. Am J Surg. 2005;190:37-38. [PubMed] [Cited in This Article: ] |
| 10. | de Bree E, Grammatikakis J, Christodoulakis M, Tsiftsis D. The clinical significance of acquired jejunoileal diverticula. Am J Gastroenterol. 1998;93:2523-2528. [PubMed] [Cited in This Article: ] |
| 11. | Liu CY, Chang WH, Lin SC, Chu CH, Wang TE, Shih SC. Analysis of clinical manifestations of symptomatic acquired jejunoileal diverticular disease. World J Gastroenterol. 2005;11:5557-5560. [PubMed] [Cited in This Article: ] |
| 12. | Svendsen CB, Hillingsø JG. [Gastrointestinal bleeding from jejunoileal diverticulosis: difficult to diagnose, simple to treat]. Ugeskr Laeger. 2004;166:3209-3210. [PubMed] [Cited in This Article: ] |
| 13. | Choi JJ, Ogunjemilusi O, Divino CM. Diagnosis and management of diverticula in the jejunum and ileum. Am Surg. 2013;79:108-110. [PubMed] [Cited in This Article: ] |
| 14. | Chugay P, Choi J, Dong XD. Jejunal diverticular disease complicated by enteroliths: Report of two different presentations. World J Gastrointest Surg. 2010;2:26-29. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 22] [Cited by in F6Publishing: 28] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 15. | Strate LL, Modi R, Cohen E, Spiegel BM. Diverticular disease as a chronic illness: evolving epidemiologic and clinical insights. Am J Gastroenterol. 2012;107:1486-1493. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 220] [Cited by in F6Publishing: 238] [Article Influence: 19.8] [Reference Citation Analysis (0)] |
| 16. | Moretti A, Spagnolo A, Mangone M, Chiesara F, Aratari A, Papi C, Koch M. [Role of rifaximin in the treatment of colonic diverticular disease]. Clin Ter. 2012;163:33-38. [PubMed] [Cited in This Article: ] |
| 17. | Tiwari A, Gupta V, Hazrah P, Lal R. A rare case of multiple jejunal diverticulosis presenting as intestinal obstruction. Clin Pract. 2013;3:e21. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |